 Principles of asepsis 1: the rationale for using aseptic technique | Nursing Times
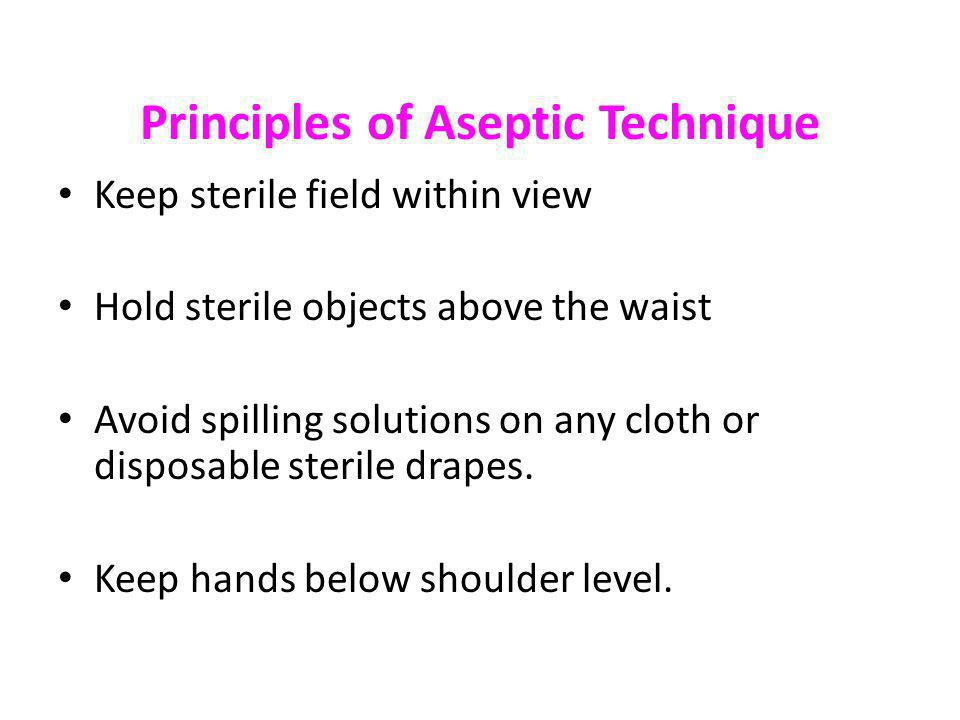
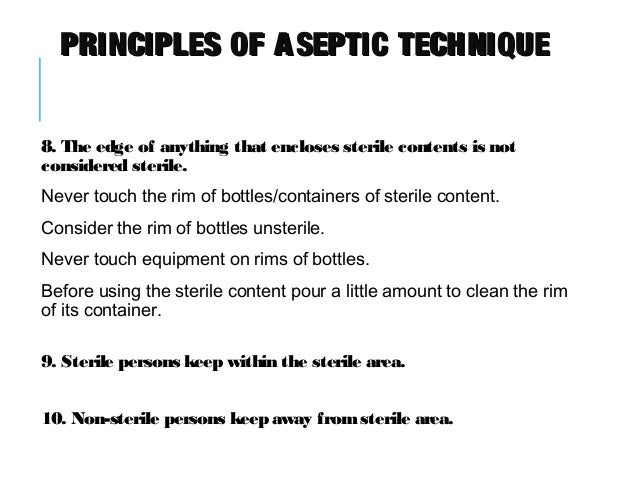
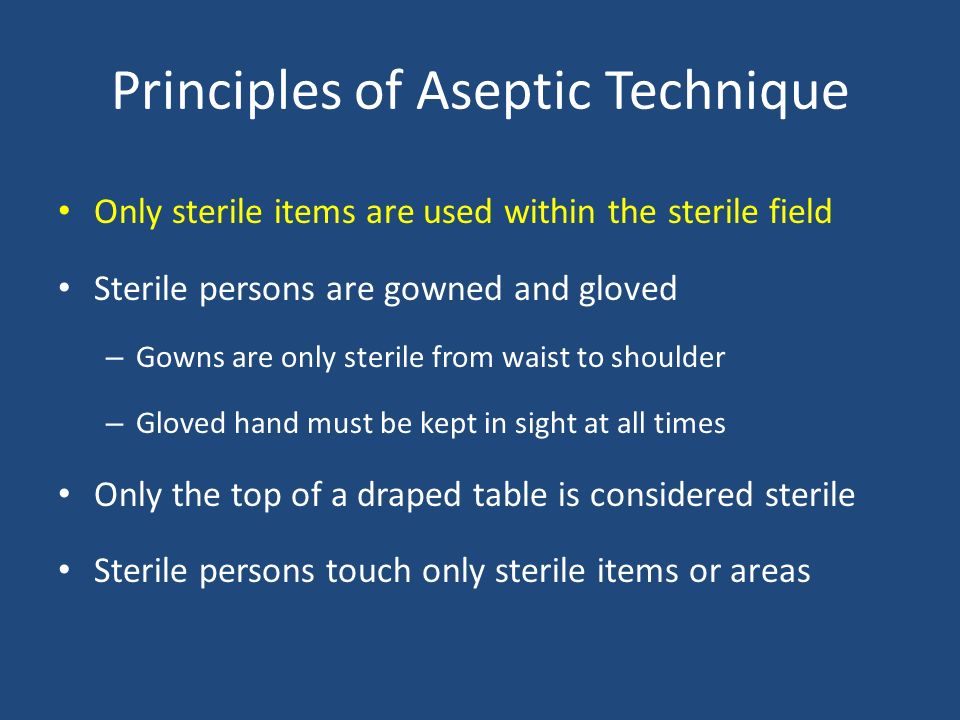
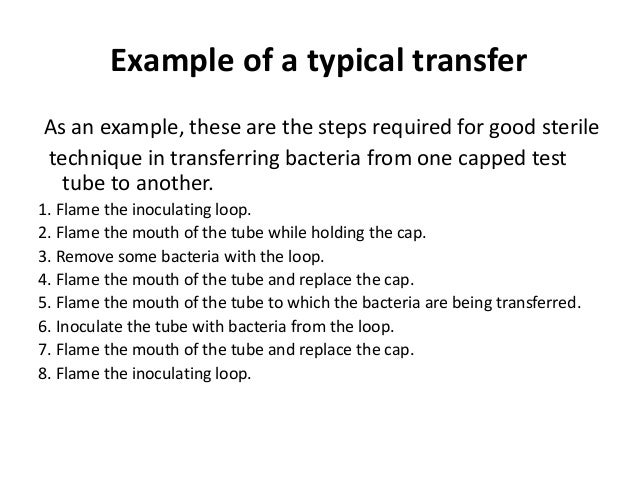
Principles of asepsis 1: the rationale for using aseptic technique | Nursing TimesPrinciples and practices of aseptic technique Aseptic technique is a method of preventing the transmission of infection to the patient during the performance of various clinical procedures. The correct practice of this technique requires the understanding of some principles and facts. BASIC FACTS RE: MICROORGANISMS " INFECTION Micro-organisms are everywhere in the environment. Since they cannot be seen with the naked eye their presence must be assumed. The infection is caused by microorganisms (Bacteria, fungi, protozoos). Some species cause infection, while others cause infection only in certain conditions and situations. However, most microorganisms are harmless. The infection depends on: The organisms can be transferred (transmitted) from one place (animate and inanimate) to another through the air, through droplets, and most importantly through contact. Agencies may be reduced in number by disinfection or completely eliminated by various sterilization methods. The interaction between factors can be represented by the equation. Factors that influence the development of the infection Factors that influence the development of the infection STRATEGIES IN INFECTION PREVENTION During the performance of the clinical procedures, the prevention of infection is done through approaches based on the above-mentioned facts. These approaches include: A single violation of aseptic technique can introduce only a small amount of microorganism and cannot lead to a serious result because small numbers can be treated by the host defense mechanism. However, multiple infractions would result in a cumulative effect that would lead to the number of bacteria reaching a significant level for the development of the infection. The development of the infection also depends on the type of organism. Another factor is the host's immunity. Immunocompromized patients (Neutropaenics), babies, elderly, diabetics and malnourished patients are especially at risk. Efforts must therefore be made to minimize the non-compliance of aseptic technique. INDICATIONS FOR ASEPTIC TECHNIQUEStrict adherence to the aseptic technique is indicated when performing invasive procedures, including the following: When a body channel or cavity normally free of microorganism (such as trachea, bronchus, urethra, bladder, ureter, renal pelvis, and calices, uterin cavity, intrascopic insertion, CSF and perpeterous When the membranes of the skin or the mucous break (surgery, insertion of IV or Arterial lines, lumbar puncture, insertion of epidural catheters) Management of traumatic and surgical wounds If a site already has resident bacteria (i.e., nose, external ear, throat, vagina), or is an infected wound; it is also important to follow (though less strict) asseptic technique in order to prevent the introduction of other more virulent organisms, especially the usual species resident in the hospital as the multi-resistent organism Staphlococcus aureus, Pseudomonas aerogenosa, Klebsiella It is composed of two areas, that is, STERILIZED INSTRUMENTS AND WORKING Concepts used in in invasive procedures are usually pre-sterilized. Sterilization eliminates all forms of microorganisms including spores. Disposable instruments are sterilized using ethylene oxide gas sterilization or gamma radiation and remain sterile in packages. Reusable items are sterilized by steam at high temperature (autoclaving) or chemical (ethylene oxide, etc.). Some instruments, for example, endoscopes, cannot be sterilized by high temperature sterilization. Low-temperature plasma sterilization technique (SterradTM) or high-level disinfectant is then used. Proprietorships are usually sterilized by gamma radiation, while the gamma is autoclaved in the Central Department of Steriles Supply at the hospital (CSSD). Disinfection and use of endoscopes in sterile body passions Endoscopes go to body cavities that do not have indigenous bacteria or are not colonized by bacteria, should be disinfected before use. These include bronchoscopes, cystoscopes, ureteroscopes, bronchoscopes and histeroscopes. Disinfection eliminates all bacteria and viruses except spores. Instruments can be disinfected using chemicals such as glutaraldehyde (CidexTM), Gigasept and peracetic acid. Disinfection should be done just before use and instrument maintained in a sterile field. It is not appropriate for these instruments to be disinfected one day in the cycloscopes or earlier. Instruments that are heavily contaminated must be sterilized. Chemical sterilization differs from disinfection in the duration of soaking, i.e. at least 30 minutes or more for sterilization instead of 10 minutes for disinfection. Otherwise, low-temperature hydrogen peroxide plasma sterilization (e.g. SterradTM) is used. The ferules, catheters and stents of biopsy should be sterile (preferably disposable). Use of Especulum " Endoscopes in Non-sterile Body Passages Instruments and endoscopes passed into body cavities that have bacteria resident or are likely to be colonized by bacteria such as mouth, vagina, nose, pharynx, external ear, esophagus, stomach, duodenum and colon, must be disinfected but not necessarily asterilized. They can be disinfected using disinfectants (glutaraldehyde [CidexTM], 70% Alcohol, Gigasept, peracetic acid, Formaldehído, Trigene, sodium hypochlorite). Once disinfected, they can be kept in a clean environment. They should not be allowed to re-contaminated, for example, by contact with an unwashed hand or dirty surfaces. STERILITY OF THE STERILE INSTRUMENTS The contamination of the sterile field will cause contamination of the instruments and other elements within it. If only gloves are used (without robes) then the rest of the body should not contact the sterile field. If the care provider carries a sterile robe, you are allowed to contact the sterile field. Sterile instruments should not be protruded. Non-sterile items should not be allowed to enter the sterile field. MINIMIZING BACTERIA AT ENTRY POINTS BY ANTISEPSIS This depends on the site where the procedure should be performed. Patient skin comas (e.g. Staphylococus epidermidis), which are harmless on the surface of the skin but may induce diseases in the blood circulation or through it to distant sites such as heart valves, urinary tract, biliary tract, lungs, or brain. When patients are hospitalized, their skin can be colonized in a short time by bacteria from the hospital environment, for example, more virulent strains of Staphylococcus aureus. The patient's skin can never be made sterile, but the amount of bacteria can be reduced by using antiseptics such as: Povidone iodine, 70% alcohol, chlorhexidena 1:200 or mixtures of these. Other surfaces including oral cavity mucosa, pharynx, nose and vagina have different sets of similar but appropriate antiseptic and resident bacteria can be used. PRACTICE OF ASEPTIC TECHNIQUE MAINTAINING THE STERILITY OF INSTRUMENTS, DEVICES & SOLUTIONS DURING TRANSPORT AND STORAGE The sterile sterilized items remain packed in wrappers, wrappers or containers. Items remain sterile if:During transfer and storage sterility you can lose if:These items should not be used. They should be sterilized again if possible. During transport, suitable carts and containers should be used. Storage areas should be kept clean, free of vermins and away from water sprays. Antiseptic solutions, including saline, must be of adequate force and not diluted (e.g. chlorohexidine 1: 2000 is ineffective). They need to have a date of use for . "In use" test (C pestS) should be done now and then. NON-TOUCH TECHNIQUE The microorganisms especially bacteria are everywhere in the environment. Its air content depends on:These facts and that bacteria can be killed by heat was known by Louis Pasteur 1887 Ref: In most clinical environments the amount and type of organisms in the air is minimal. As such, exposure of objects to the air during clinical procedures is not considered as pollution and does not cause them to lose their sterility. However, contact with any other non-sterilized object makes the instrument or article unsterile. Therefore, the most effective way to maintain sterilized instrument sterilization and other elements is non-touch technique. In this technique work processes are developed so that the sterile or disinfected element does not contact non-sterile elements. This can be achieved by considering possible cases in which pollution can occur in the context of various procedures and by developing methods to avoid it. The technique does not touch ensure that the instruments or articles remain sterile during a procedure. When packets/ envelopes are opened, it ensures that the inside of the package is not touched. Transfer the item or the pack inside the package to the sterile field, either by dropping it, by holding it with a hand / sterile armchairs gloves without touching the outside of the package. Full sterile instruments / disposable items (such as lines and catheters) must be inside a sterile field. If a non-sterile instrument should be used during the procedure, then the sterile sleeves or the sterile see through the decks should be used (axill probe microscopes, button switches). MAINTAINING STERILITY OF THE GLOVED HAND Sterile gloves are used to render the sterile of the hand as washing the hands with antiseptic will only reduce the number of bacteria in it. Hand wash remains an essential part of aseptic technique because gloves can have inherent holes or be drilled during the procedure. Therefore, hand washing according to the accepted procedure is mandatory especially when surgery is performed. For the first case for the day, rub your fingers and nails with a soft brush until it is clean. Wash your hands to elbow, preferably with Propyl alcohol plus chlorohexidine or iodine Povidone, for 5 minutes. For subsequent cases a 2-3 minute hand wash until the elbow is sufficient. There is no need to scrutinize the forearms. In practice it is very easy for the beautiful hand to be re-contaminated unless strict precautions are taken. Some include: ASEPTIC TECHNIQUE IN VARIOUS SITUATIONS PROCEDURES OF WORK IN A When working alone, perform tasks that do not require a sterile hand first before entanglement. For example, when preparing sets / instruments for a procedure opens the set, creates the sterile field and puts first into additional articles or lotions. Open the outer envelope of the glove pack completely before washing the hand. When a hand is required to perform a task that requires contact with an unsterile object or surface, consciously identify the contaminated hand and perform procedures with the other hand. Common situations include:Urinary catheterization Hold separate minor labia or slide the penis prey with the non-dominant hand (usually left). Clean the urethral opening with antiseptic and insert the catheter with the dominant sterile hand. Performing Laryngeal Suction in a Patient with Tracheostomy Hold the non-sterile sucker tube with the left hand and the sterile suction catheter with the right hand. Disconnection " Reconnection IV/Artistic Pollution of cannules and lines can lead to the sepsis line. This is unlikely if cannules are kept for short periods (no ±48 hours). However, central lines, femoral lines and umbilical artery catheters pose a greater risk than in turn can cause systemic sepsis or infection in distant sites. In neonates, a possible distressing complication is septic arthritis and osteomyelitis in metaphisis. The connector takes the form of a Luer lock with the tip of the line being male while the cannula bridle is female. The inside of the tip of the line should remain sterile. The entire flange of the canula must remain sterile. To disconnect, grab the base of the canula firmly, oclude the vein or artery with a finger and unmask the tip of the line with the other hand. The tip should remain sterilized by holding it in the air hanging on the drip holder with the help of a pre-prepared tape or asking the patient to keep the line short distance from the tip. Place a spur or a plug in the cannula flange. A needle or a pod jet is used to oclude and cover the tip of the infusion line. To reconnect, remove the needle or push from the tip of the line. Then hold the base of the cannula firmly and remove the sprinkler or the plug. Step back the tip of the line in the cannula flange. In fact, it is very difficult to prevent contamination during this procedure when it is performed by a single individual. It's better if it's made by two people. PROCEDURES WHERE at LEAST TWO PERSONS MUST INVOLVED Many procedures should be performed by at least two people if asepsis is reached: one (or more) performer within the sterile field, and another assistant/partner working outside the sterile field. The practice of aseptic technique during some of the most common procurements is discussed below. Surgery – Minor and Major (operational team and circulating nurse)Indoscopic therapeutic processes (performer and assistant)Edotracheal intubation with an ET tube The first performs direct laryngoscopy with a larynxoscope and identifies the opening of the glyotis. The attendant must open the ETT sterile package completely. The interpreter collects the outer end of the tube and inserts the inner end directly into the trachea without touching structures in the mouth and throat (you should not bend the tube at the bare OT table!). If for any reason the ETT tube needs to be put down, put it back in the sterile package cared for by the attendant. Insertion of a central line (performer and assistant). The assistant introduces the cannula IV and all connection tubes into the sterile field. Before the interpreter has inserted the cannula, passes the end of the intravenous pipe (used to puncture the IV solution bag) to the attendant. The wizard connects the tube to the bag and the fluid runs on the main line. The other end remains sterile in the sterile field and the interpreter connects it to the intravenous cannula inserted. Insertion of chest Drains, Peritoneal Dialysis " Catheter urine The attendant places all tubes and containers in the sterile field using a non-touch technique. The person who inserts the tube must secure the connections before passing the containers (subbaquatic seal bottles / urine containers / dialysis bags) to the attendee. Problems arise when the sterile catheter or tubes need to connect to connectors outside the sterile area. In that situation the sterile end (woman) is passed to the assistant who will connect it to the connector (man) who has remained sterile. Performing Tracheo-Bronchial Suction in a Ventilated Patient The aseptic technique is possible only if two care providers perform the task. A person disconnects and reconnects the ventilation tube or the Ambu bag to the endotracheal tube/tracheostomy. The other person performs suction with a sterile catheter using both hands gloves. When delivering babies The risk of puerperal sepsis is always present (as at the time of Semmelweis in 1847 Ref: ). Normal spontanea delivery can be performed by an obstetric or median woman, but for instrumental delivery (vacuum removal or forceps) at least two people are required. The instrument pack when opening should cover a whole cart and more. The skin of the perineum and the groin should be cleaned with Cetrimida 3% or Chlrohexidine aqueous 1:200. Ref: . The obstetrician should wear a sterile robe. You need to remove the patient with sterile leaves that expose only the perineo and the introitus. Manage the baby (resurrection and so on) must be a separate procedure of childbirth itself. Perform the wound yarn and dress. It's customary to name both parties as a clean nurse and a dirty nurse. Maybe it's better to call them inside the nurse and outside the nurse, that is, inside and outside with respect to the sterile field. The outer nurse opens the outer cover of the dressing set. The inner nurse washes her hand and wears a couple of sterile gloves. Open the inner layer of the wrap using your hands or the forceps provided. The outside nurse now leaves pieces of gauze, cotton hisopos, syringe and scissors in the sterile field created and after which she spills lotions in the galley pots. Then proceeds to remove the existing external deposit in the wound. The inner nurse should remove the deposits inside the wound with a couple of sterile forceps that passes outside. Then clean the skin around the wound with 70% alcohol or chlorohexidine. The edge and base of the wound are cleaned with the Chlorohexidine 1:200 solution. If the MRSA is present you should use the Povidone iodine and if it is Pseudomonas, it is usual to use acetic acid. Sodium hypochlorite and hydrogen peroxide can be used for obviously infected wounds. The wound is completely red with sterile saline or water using a syringe. At the early stage of the wound-care gauze soaked in the right antiseptic mentioned above or filled with the patented antiseptic wound can be left inside the wound. The dry gauze or the patented dressing is used for the external dressing and is fixed with any type of plaster or a transparent dressing cover can be used. When the wound is removed from the infection, wet gas is used with the saline dressing or the patented smooth. Otherwise, no gauze is placed in the wound, but a dressing foam or adhesive plastic roof is placed on the wound and left untouched for two or more days. CONCLUSION The practice of aseptic technique requires an understanding of the principles involved, adherence to appropriate procedures, the use of adequate resources and an appropriate environment. While monitoring and monitoring are essential, compliance can only be achieved through individual commitment and attention to detail. Share this: Thus: 10 thoughts on "Principles and practice of aseptic technique" Esther sule Thank you for the wonderful writing. Do you want to ask if it's aseptico also known as sepsis? Like Thanks for reading my article. Asepsis means "no sepsis" or. a situation in which pathogens (microorganisms) have not been introduced. I suppose the aseptic technique is the way to establish the condition of asepsis. LikeEJThank you for this article on aseptic technique Dr. Salleh. I believe that these principles should be disseminated and applied by the public, especially with the current COVID-19 pandemic. The only challenge that exists about how to implement and inculcate these principles to our current and future people, as we all know that this aseptic technique is usually only made by nurses and everyone in the medical field, not in normal situations by normal people. Like Thanks for your comments. We can start with the food industry. Food packing and franchising industries are quite good but restaurants and ordinary hawks do not understand food hygiene. For Covid-19 the regular cleaning of the surfaces frequently touched by people needs more attention. Like Daddy Thank you. Dr for your support in facilitating a better understanding of aseptic technique and principles. I have a question. in a case that you as an inner nurse who performs the dressing procedure and the outside nurse or the dirty nurse passed to the pure asptic solution on the sterile work surface, is the sterility of the aseptic procedure still maintained or not? As antiseptic solutions are used to kill bacteria and are intended to be applied to wounds. They don't contaminate the sterile field. When fresh, solutions do not contain bacteria. However, the rest in the bottle/container can be contaminated after some time. If a solution is dispensed in a large and reused container many times, a test of culture and sensitivity in use should be made. If there is bacterial growth, it must be discarded. The best way would be to get from the pharmacy or buy from suppliers antiseptic solutions contained in small bottles/containers sufficient for use once or twice (in one day or two). LikePRISCA Oluchi Ulu Thank you, Doctor for this wonderful writing. Please, for reference purposes when did you publish this? Like Thanks for the interest. I wrote it for the first time on August 4, 2014. It has been updated, being the last !9 June 2017. Abdollah Salleh On Sat, 7 Jul, 2018 at 5:08 AM, Health Care Service Delivery wrote: √≥Like I wrote it for the first time on August 4, 2014. It has been updated, the last is June 19, 2017. As I should point out my admiration for your kindness by supporting individuals who must have help with this particular issue. His own dedication to passing the solution all over the world came to be quite functional and have consistently helped guys like me achieve their goals. Your own invaluable information involves a lot of people like me and even further away from my peers. Thank you; all of us. How toLeave a Comment Fill in your data below or click on an icon to log in: You are commenting using your WordPress.com account. (sighs) ) You're commenting using your Google account. (sighs) ) You're commenting using your Twitter account. (sighs) ) You're commenting using your Facebook account. (sighs) ) Connect to %s Notify me of new comments by email. Notify me of new email messages. This site uses Akismet to reduce spam. .Internet > Dr. Blog. Abdollah Salleh Blog via e-mail Enter your email address to follow this blog and receive notifications of new posts by e-mail. E-mail: LicenseCreative Commons Attribution-NonCommercial International License 4.0. Blog StatsAuthor I am a retired surgeon who currently offers consulting services in Information Management in Health Services. My interests and experience have been in patient care, quality management, clinical governance, medical education and information management (among other things). From 1977 to 2011 he served as a physician in primary, secondary and tertiary care with the Ministry of Health of Malaysia. I am a member of Malaysian society for quality in health, Malaysia; a society that I helped establish and be a hospital accreditation surveyer for many years. I have been a visiting professor and taught graduate and graduate students at various medical colleges (UITM, UKM and USM) in Malaysia. At Selayang Hospital, Malaysia, I was Chairman of the Clinical Advisory Committee, Clinical Coordinator and Quality Coordinator for almost 10 years. I have helped implement computer hospital information systems in several hospitals. I graduated with MBBS from the University of Malaya in 1977. I was (but since then it has ceased to be) a companion for examination of RCS Edinburgh and RCPS Glasgow. I am contactable by email to: drdollah@gmail.com License The content of this website is licensed. The articles can be freely copied or reproduced attribution to the author. Permits beyond the scope of this license are available by e-mail: drdollah@gmail.com
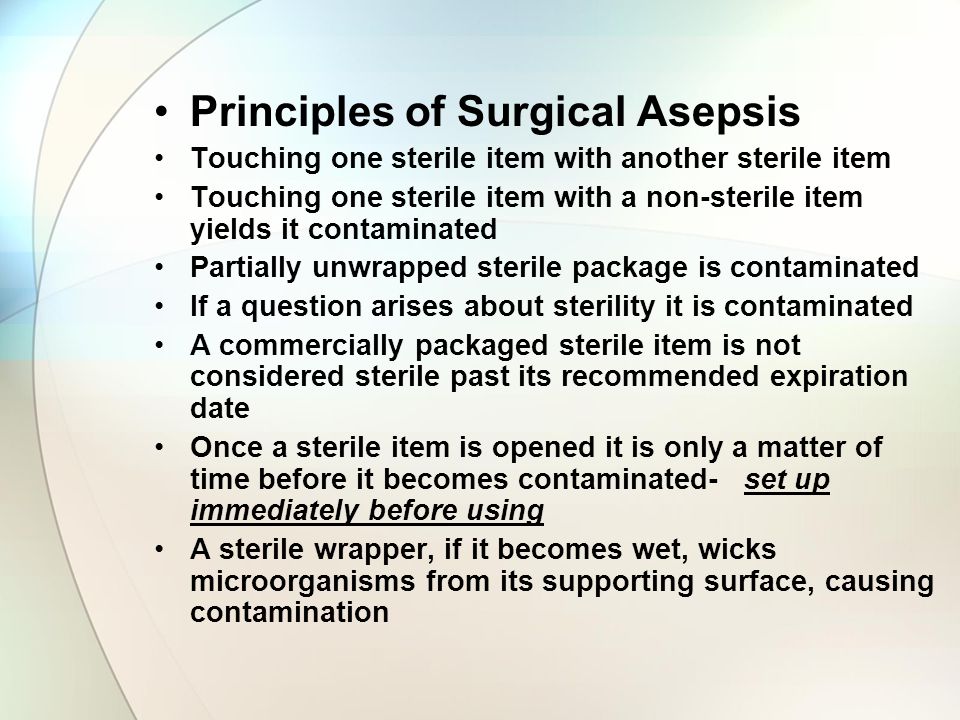
OR WAIT null SECS © 2021 MJH Life Sciences and Infection Control Today. All rights reserved.© 2021 MJH Life SciencesTM and Infection Control Today. All rights reserved. Asepsis and aseptic practices in the operating roomAsepsis and aseptic practices in the operating room by Cathy Osman, RN, BSN, CNORThe prevention of surgical infection in the operating room is the main objective of the surgical team, and all activities carried out by the team support this objective. Some of these activities include patient risk assessment, environmental cleaning, disinfection and sterilization of the instrumentation, the patient's antibiotic prophylaxis and the use of standard precautions. However, the activities of aseptic-related O.R.s and aseptic practices have the greatest direct impact on the surgical team to help reduce the risk of the patient to the surgical infection of the site. The goal of asepsia is to prevent contamination of the open surgical wound by isolating the operating site of the surrounding non-sterile environment.1 The surgical team manages to create and maintain the sterile field and following aseptical principles aimed at preventing microorganisms from contaminating the surgical wound.3 The recommended rules and practices, developed by the Association of Peripheral Registered Nursing (AORN), are guidelines that the surgical team should use to achieve the optimal level of technical and aseptic practice by caring for their patients in the perioperative environment3. These guidelines should not be considered political. Institutions should use them to provide guidance and information on perioperative practice, as they incorporate them into their own policies and procedures. The principles of aseptic technique play a vital role in achieving the goal of asepsis in the operating environment. It is the responsibility of each surgical officer to understand the meaning of these principles and to incorporate them into their daily practice. The principles of aseptic technique include the following principles. Principle #1Scrutinized people work within a sterile field. 2 The surgical team is composed of sterile and non-sterile members. The sterile members or the staff "heard" work directly in the surgical field while non-sterile members work on the periphery of the sterile surgical field. All members of the surgical team wear scrub suit. In addition to scrub dress, scrub people should wear a sterile surgical dress, mask and gloves inside the sterile field to establish bacterial barriers. 2.4 These barriers protect the patient from the transmission of microorganisms from the surgical equipment. Once the scrubbed person donates the sterile surgical dress, the sterility of the dress is limited to portions of the robe that the scrub person sees directly. These sterile areas include the front of the robe, from the chest to the sterile field level, and the two-inch sleeves above the elbow to the fist. 2,4 The scrub staff always performs a surgical hand scrub before donating their sterile surgical dress and gloves. Principle #2Sterile curtains are used to create a sterile field. 2.5Sterile surgical curtains establish an aseptic barrier minimizing the passage of microorganisms from non-sterile areas to steriles.2 The sterile curtains should be placed in the patient, the furniture and the equipment that will be included in the sterile field, leaving only the exposed incisional site.5 During the damping process, only scanned personnel should handle sterile curtains. The curtains should be held higher than the operating room with the patient wrapped from the prepaid incisional site to the periphery. 2 Once the sterile drape is placed, it should not be moved or reorganized.5 Please note that after the patient's and O.R.'s tables are wrapped, only the upper surface of the covered area is considered sterile. 1Principle #3All elements used within a sterile field must be sterile. 2.4 2.4 In no case should sterile and non-sterile items be mixed, as one contaminates the other.4 Sterilization provides the highest level of security that all instruments, sutures, fluids, supplies and curtains do not have microorganisms.2 The sterility of a package is determined by events, not by time. In order to ensure sterility, all sterile elements need to be inspected for the indicators of the process of integrity and sterilization of packages, such as the indicator tape and internal chemical indicators, before being introduced in the sterile field.2 If a package has been compromised, it should be considered contaminated and not used. 5Fluid or air can contaminate a sterile package. When the liquid enters a sterile package, a fluid attack occurs. The fluid creates a vehicle in which the migration of microorganisms reaches the sterile element. When a sterilized item falls on the ground, the air penetrates the sterile package. The force that is created when the package is contacted with the soil can cause the sterile barrier to penetrate by forcing the sterile air and allowing the contaminated air and particles in the package.1.3Principle #4All elements introduced in a sterile field must be opened, dispensed and transferred by methods that maintain sterility and integrity. 2.4 All sterile items must be dispensed to the sterile field by methods that preserve the integrity of the articles and the sterile field.1 Non-sterile staff, usually the circulating nurse, should use a good trial by dispensing sterile items on the sterile field, either by presenting them directly to the person scrutinized or by placing them safely in the sterile field.1.2 The sterile items that are thrown on the sterile field can move other sterile items, penetrate the drape, or release the fertile rolled first. The last wrapper flap is thrown into the non-sterile person who opens the package.3 This technique of opening a package wrapped ensures that the non-sterile person does not reach the sterile element inside. All wrapping edges should be secured to avoid turning the wrapper and contaminating the contents of the sterile package or field. 2.5 After a wrapper has been opened, the inside of the wrapper and its contents are considered sterile except for the outer edge of 1 inch of the wrapper.1 This 1-inch outer edge of the wrapper is considered the "safety margin" between sterile and non-sterile. When a package is double-involved, the policies and procedures of each institution determine whether one or both wrappers open before they are presented to the sterile field. 5 When opening a packet of peel, the non-sterile person opens the package by rolling the wrap on his hands and presenting the internal contents of the package to the scrutinized person.5 The package and its contents should be presented in such a way as to prevent contamination of the sterile item or the scrutinized person. When determining the sterility of the package content, the inner edge of the heat seal is considered the line that separates sterile from non-sterile. When opening a solution container, the non-sterile person should lift the lid directly and pour the contents of the bottle into a sterile container. The sterile container is maintained by the person cut out of the sterile field or placed near the edge of a table resistant to sterile water. Only the top edge of the top of the bottle and the contents of the bottle are considered sterile once the lid has been removed from the bottle. Therefore, when sterile fluids are dispensed, all the contents of the bottle or the remaining liquid in the discarded bottle should be poured.1 When the solutions are poured into the sterile field, they must be poured slowly to prevent contamination and fluid strike from coming out. 2Principle #5A sterile field must be maintained and monitored constantly.2,5 It is the responsibility of the staff of the operating room to monitor and maintain the sterile field. Sterility can never be absolutely guaranteed, but members of the surgical team must make reasonable efforts to reduce the likelihood of contamination and be vigilant to sterility violations.2 When a sterility violation occurs, team members must take immediate and appropriate measures to correct the breakdown in the technique to reduce the additional risk of contamination. Remember, if there is doubt about the sterility of an article, consider that it is not sterile.3 The sterile field should be prepared as close as possible at the time of use.2 The sterility of the supplies used during a surgical procedure may be affected by the events occurring in the O.R. and the length of time the articles have been exposed to the environment.4 Once established, the sterile field must be constantly monitored. When the sterile field is left unattended, staff, air pollutants, insects and liquids can contaminate the sterile field.2 Each facility must have policies and procedures that address these problems so that the surgical team will follow. Principle #6 All the staff that moves inside or around a sterile field must do so to keep the sterile field. 2 As the patient is the center of the sterile field, the staff must remain close to this area without wandering through the room. This movement can result in contamination of the sterile field. 2.4 Scrub personnel must move from sterile areas only to sterile areas. When the search staff changes position, it should keep a safe distance between itself and always pass one to the other by turning back to the back or face to face.2 This movement reduces the risk of contamination by ensuring that people of scruples are passing non-sterile to non-sterile or sterile. The search staff must remain in the position in which the surgery began. For example, if the surgery begins with the scrutinized person sitting and is completed with the scrutinized person standing, the part of the dress that was considered sterile is uncertain.5 The search staff must keep their arms and hands inside the sterile field at all times to avoid any accidental contact with items or non-sterile areas. The search staff must maintain a safe distance by approaching non-sterile objects and personnel. This safe distance or "security margin" is important to identify safe limits between sterile and non-sterile areas. Non-sterile personnel should always remain in non-sterile areas and contact only non-sterile items to prevent sterile contamination. It is important that non-sterile staff always face the sterile field on the approach and should never walk between two sterile fields.2 This ensures that the sterile area is always observed and accidental contact is avoided. Like the sterile scrub should maintain a safe distance from areas and non-sterile people, non-sterile staff should always be aware of and maintain a "safety margin" by approaching sterile fields and scrub staff. And finally, when you deliver sterile supplies to the sterile field, the non-sterile team member must always maintain a "safety minimum" between them and the sterile field, never contact or get anywhere in the sterile area.5 This "safety margin" is usually identified at least 12 inches (30 cm) or more. Principle #7 Policies and procedures for maintaining a sterile field should be written, revised annually and readily available in the practice environment. 2These best practices for aseptic technique should be used as guides to develop policies and procedures within the practice environment. 2 The introduction and review of policies and procedures should be included in the orientation and ongoing education of all peri-operative personnel. 2Training of aseptic technique and practices requires experienced and qualified surgery team members to demonstrate these skills to new and inexperienced personnel. A new staff should be assigned an experienced mentor who will be a good role model and a teacher who provides leadership and education in perioperative practice. Abstract All members of the surgical team must practice these aseptic techniques principles to help prevent the transfer of microorganisms to the surgical wound during the perioperative period. It is the responsibility of the members of the surgical team to develop a strong surgical consciousness, adhering to the principles of asepsia and rectifying any inappropriate technique that has been a witness in the O.R. In addition to the principles of asepsis, the proper surgical outfit plays an important role in reducing the surgical infections of the site by reducing the amount of hair and skin contaminants reaching the sterile field. The objective of asepsis and aseptic technique is to prevent the transfer of microorganisms to the surgical wound. Preventing the surgical contamination of the site requires the efforts of all members of the surgical team trained to use their knowledge and experience in aseptic practices to provide their patients with optimal care resulting in positive surgical results. For references, access the ICT website. Related Content: Related Content:
Principles OF Aseptic Techniques - StuDocu
principles of Aseptic
ANTT | PHA Infection Control
AsepticTechnique
Chapter 15: Principles of Asepsis and Sterile Technique by Natalie Davis
13 Principles of Sterile Technique | Nature
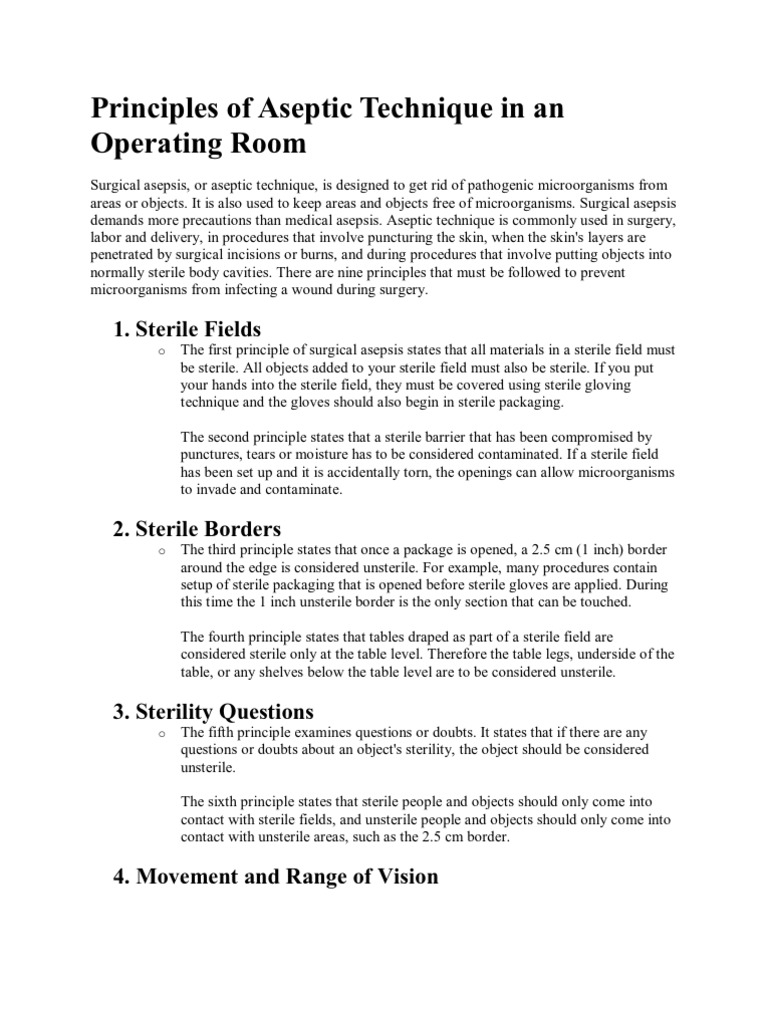
Principles of Aseptic Technique in an Operating Room | Surgery | Public Health
Learning Plan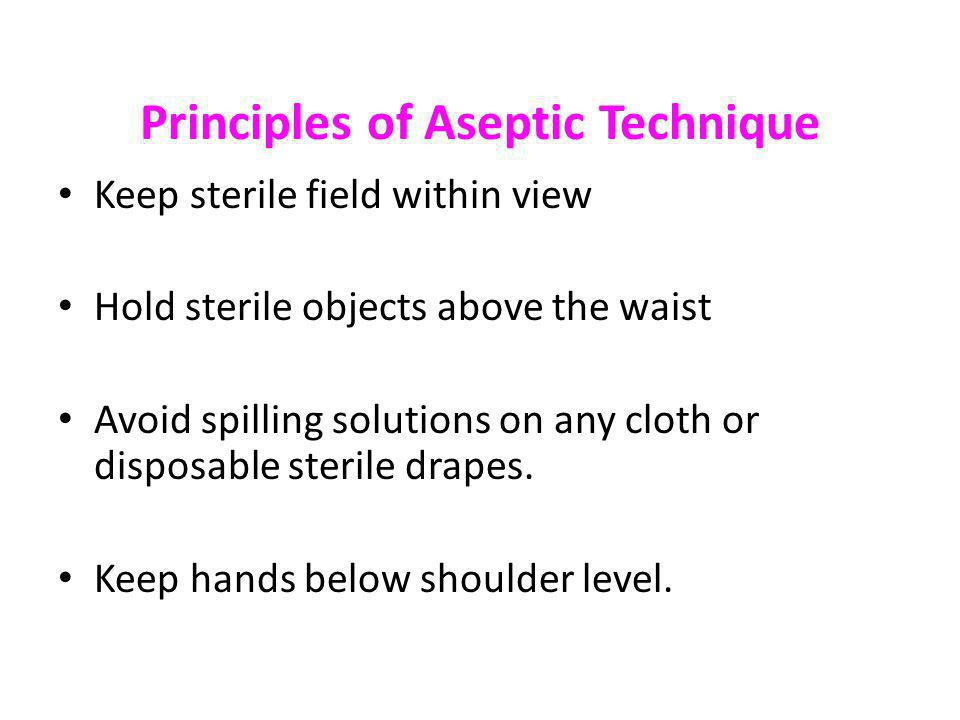
Unit Aseptic Techniques - ppt video online download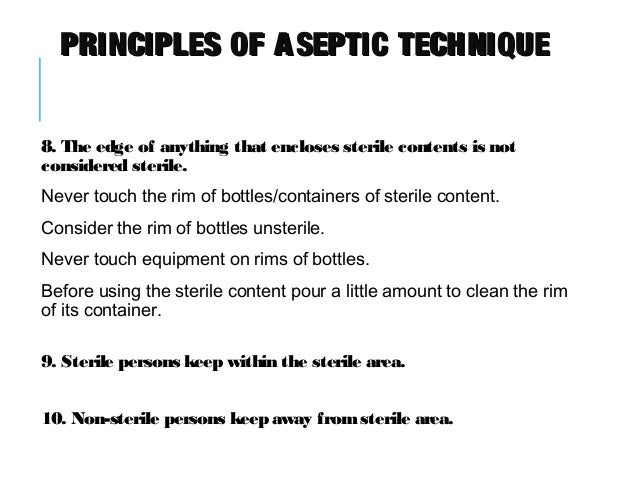
principles of Aseptic
Surgical Asepsis in the OR - ppt video online download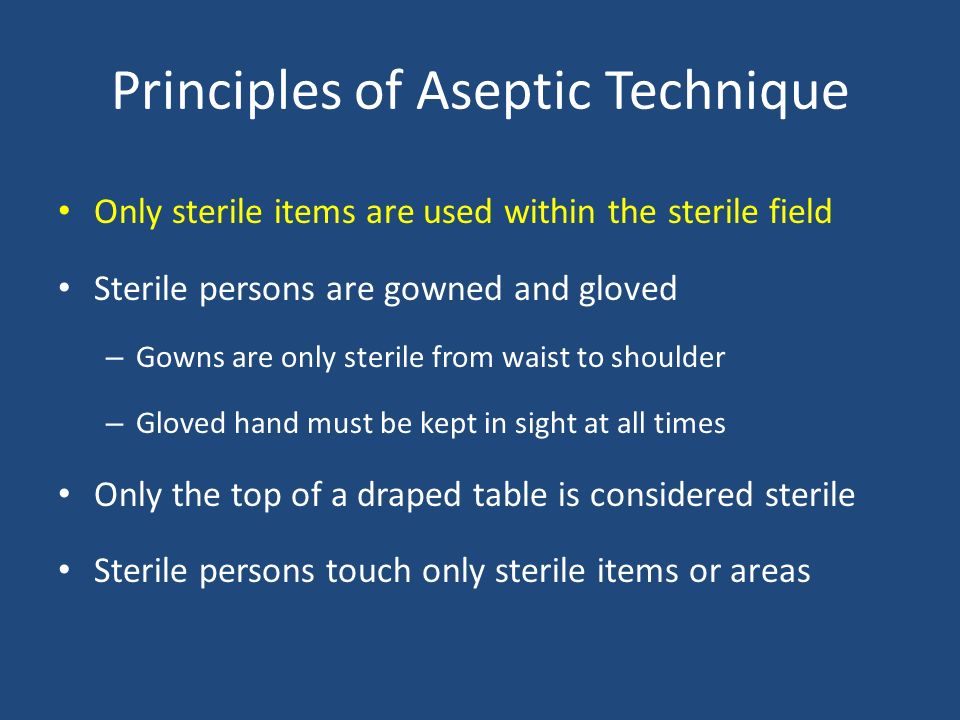
Surgical Asepsis in the Operating Room (OR) By Dr. Iobey. - ppt download
Principles of asepsis 2: technique for a simple wound dressing | Nursing Times
ANTT | PHA Infection Control
Aseptic technique Essentials for animal research: A primer for research personnel, 2nd Edition, Chapter 5 - Principles of Aseptic Technique, John C. Schofield, B.V.Sc., M.R.C.V.S. Adapted from: Sli
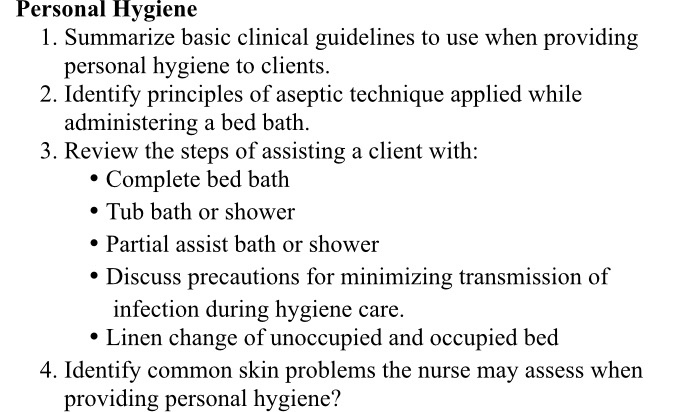
Solved: Personal Hygiene 1. Summarize Basic Clinical Guide... | Chegg.com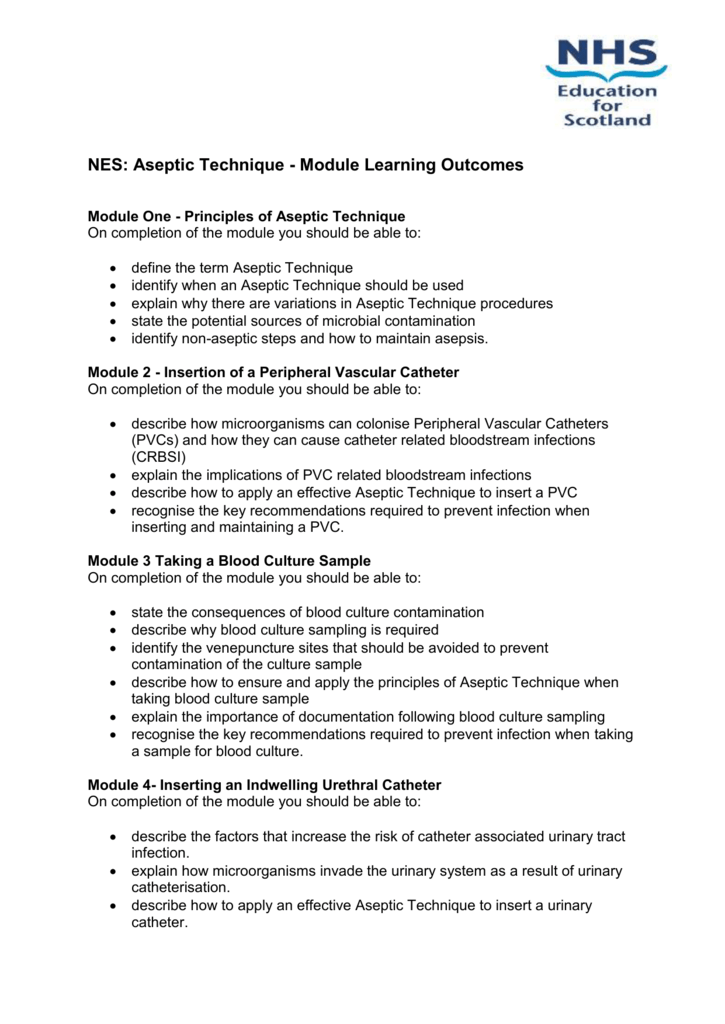
Aseptic Technique Module Learning Outcomes
Principles of Asepsis. - ppt download
Aseptic technique
principles of aseptic technique
Principles of Aseptic Technique | Glove | Surgery![Aseptic Dressing Technique 1 - .Aseptic Dressing Technique 1 CETL 2008 Three principles of aseptic - [PDF Document] Aseptic Dressing Technique 1 - .Aseptic Dressing Technique 1 CETL 2008 Three principles of aseptic - [PDF Document]](https://demo.fdocuments.in/img/742x1000/reader019/reader/2020041411/5b903d0909d3f252108b6d6f/r-1.jpg?t=1610221161)
Aseptic Dressing Technique 1 - .Aseptic Dressing Technique 1 CETL 2008 Three principles of aseptic - [PDF Document]
Principles and Practices of Asepsis - ppt download
Note on Concept of asepsis
Principles of asepsis 1: the rationale for using aseptic technique | Nursing Times
Aseptic Technique - Goals and Objectives
Principles of Surgical Asepsis - Nursing Crib
Principles of asepsis 1: the rationale for using aseptic technique![ASEPTIC TECHNIQUE[1] |authorSTREAM ASEPTIC TECHNIQUE[1] |authorSTREAM](https://lh3.googleusercontent.com/blogger_img_proxy/AEn0k_tyoyLZnEkMRoA2BSe-ZOGrj2PLtJX3Z4PWRGZgnoQw8BVMDDDGYObYRCuEZXjpcwF3M6zaSCtvLVhuCAv6S4kaB8GlL3u6oheKwLxT8PKbxIrd-xMLKb82fddHVADHOLQ=s0-d)
ASEPTIC TECHNIQUE[1] |authorSTREAM
PDF) Sterile versus non-sterile glove use and aseptic technique
Surgical Asepsis – Principles and Aseptic Practices, Medical Asepsis - Aseptic Practices and Disinfection of Articles
Aseptic Processing & PPE. Two Broad categories of contamination: Non-Viable & Viable - Non-viable particulate contamination is defined as a solid or. - ppt download
Princilples of aseptic
Principles of Asepsis and Sterile Techniques | Transmission (Medicine) | Infection
Principles of asepsis - Week 1 - YouTube
NES: Aseptic Technique - Module Learning Outcomes
Lesson 4 st.docx - epacia oli Lesson 4 Principles of Aseptic Technique Exam A patient is infected with Staphylococcus aureus and Escherichia coli at the | Course Hero
ASEPTIC TECHNIQUE || PRINCIPLES || OPERATING THEATRE || NURSING KNOWLEDGE - YouTube![Principles Of Aseptic Technique In An Operating Room [m34m51jdxmn6] Principles Of Aseptic Technique In An Operating Room [m34m51jdxmn6]](https://idoc.pub/img/crop/300x300/m34m51jdxmn6.jpg)
Principles Of Aseptic Technique In An Operating Room [m34m51jdxmn6]
Surgical Asepsis Chapter ppt download
 Principles of asepsis 1: the rationale for using aseptic technique | Nursing Times
Principles of asepsis 1: the rationale for using aseptic technique | Nursing Times









![Aseptic Dressing Technique 1 - .Aseptic Dressing Technique 1 CETL 2008 Three principles of aseptic - [PDF Document] Aseptic Dressing Technique 1 - .Aseptic Dressing Technique 1 CETL 2008 Three principles of aseptic - [PDF Document]](https://demo.fdocuments.in/img/742x1000/reader019/reader/2020041411/5b903d0909d3f252108b6d6f/r-1.jpg?t=1610221161)






![Principles Of Aseptic Technique In An Operating Room [m34m51jdxmn6] Principles Of Aseptic Technique In An Operating Room [m34m51jdxmn6]](https://idoc.pub/img/crop/300x300/m34m51jdxmn6.jpg)
Posting Komentar untuk "principles of aseptic technique"