side effects of castration
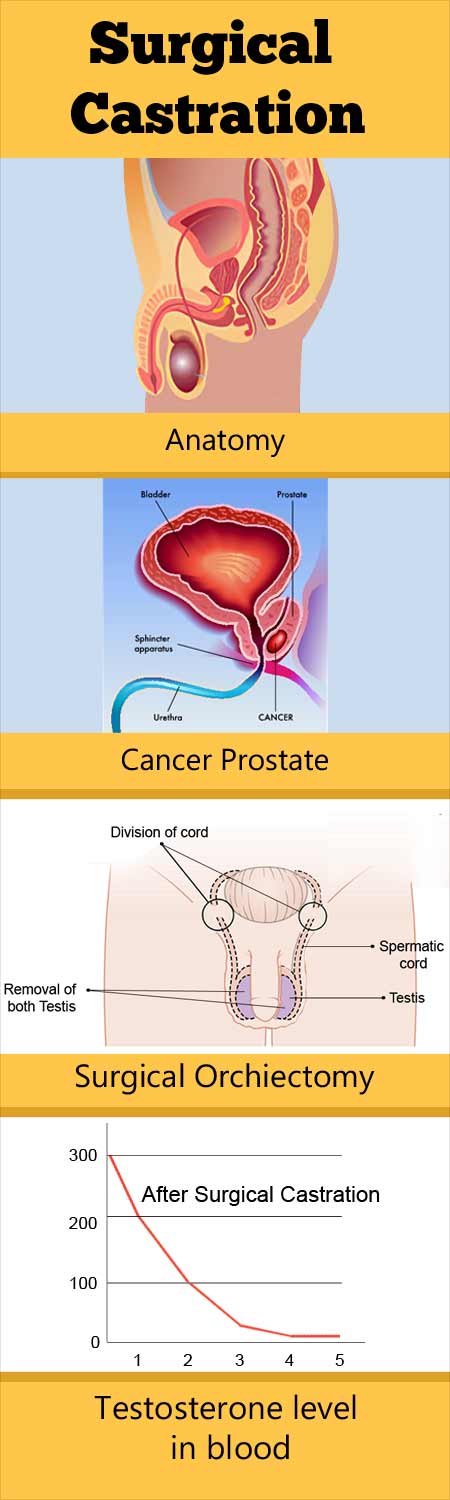 Surgical Castration
Surgical CastrationNo resultsNo resultsProcessing results.... What are the adverse effects of surgical and medical castration on the treatment of prostate cancer? Surgical and medical castration leads to a series of side effects, including the following, which can have a significant impact on a man's quality of life: Related questions:Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN estimates the incidence and mortality worldwide by 36 cancers in 185 countries. CA Cancer J Clin. 2018 Nov. 68 (6):394-424. . American Cancer Society. Cancer data " Figures 2021. Available in . Access: February 2, 2021. Shah, Rajal B., and Ming Zhou. Isthological variables of Adenocarcinoma Acinar, Ductal Adenocarcinoma, neuroendocrine tumors and other carcinomas. Interpretation of prostate biopsy. 2019. 69-95. Humphrey PA, Moch H, AL, Ulbright TM, Reuter VE. WHO 2016 Classification of Urinary System Tumors and Male Genital Organs Part B: Prostate and bladder Tumors. Eur Urol. 2016 Jul. 70 (1):106-119. . Merriel SWD, Funston G, Hamilton W. Prostate cancer in primary care. Adv Ther. 2018 Sep. 35 (9):1285-1294. Thompson IM Jr, Leach RJ, Ankerst DP. Focusing PSA High-strength prostate cancer screening tests incorporating patient preferences in decision-making. JAMA. 2014 Aug 4. Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, et al. A contemporary prostate cancer classification system: an alternative validated to the Gleason score. Eur Urol. 2016 Mar. 69 (3):428-35. . Haas GP, Delongchamps N, Brawley OW, Wang CY, of the G Roza. Global epidemiology of prostate cancer: prospects for autopsy studies. Can J Urol. 2008 Feb. 15 (1):3866-71. . Sánchez-Chapado M, Olmedilla G, Cabeza M, Donat E, Ruiz A. Prevalence of prostate cancer and prostatic intraepithelial neoplasia in Caucasian Mediterranean males: an autopsy study. Prostate. 2003 Feb 15. 54 (3):238-47. Crawford ED. Understand epidemiology, natural history and the key pathways involved in prostate cancer. Urology. 2009 May. 73 (5 Suppl):S4-10. . Etzioni R, Tsodikov A, Mariotto A, Szabo A, Falcon S, Wegelin J, et al. Quantify the role of PSA detection in reducing prostate cancer mortality in the United States. Control of Cancer Causes. 2008 Mar. 19 (2):175-81. . Howrey BT, Kuo YF, Lin YL, Goodwin JS. The impact of PSA screening on prostate cancer mortality and overdiagnosis of prostate cancer in the United States. J Gerontol A Biol Sci Med Sci. 2013 Jan. 68 (1):56-61. . van Leeuwen PJ, Connolly D, Gavin A, Roobol MJ, Black A, Bangma CH, et al. Mortality of prostate cancer on screen and prostate cancer clinically detected: estimation of the benefit of detection. Eur J Cancer. 2010 Jan. 46 (2):377-83. Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019 Apr. 10 (2):63-89. . Disease data: Prostate cancer. National Cancer Institute. Available in . Access: February 2, 2021. Weiner AB, Matulewicz RS, Eggener SE, Schaeffer EM. Increase the incidence of metastatic prostate cancer in the United States (2004-2013). Prostate Cancer Prostatic Dis. 2016 Jul 19. . .Bleyer A, Spreafico F, Barr R. Prostate cancer in young men: A young and older adolescent challenge. Cancer. 2019 Sep 25. O'Keefe EB, Meltzer JP, Bethea TN. Health and Cancer Disparations: Racial Disparities in Cancer Mortality in the United States, 2000-2010. Frontal Public Health. 2015. 3:51. Pernar CH, Ebot EM, Wilson KM, Mucci LA. The epidemiology of prostate cancer. Cold Spring Harb Perspect Med. 2018 Dec 3, 8 (12): Barber L, Gerke T, Markt SC, Peisch SF, Wilson KM, Ahearn T, et al. Family history of breast or prostate cancer and risk of prostate cancer. Clin Cancer Res. 2018 Dec 1. 24 (23):5910-5917. . Giri VN, Knudsen... Wender R, Gomella LG. Role of Genetic Testing for Inherited Prostate Cancer Risk: Philadelphia Consensus Conference on Prostate Cancer 2017. J Clin Oncol. 2018 Feb 1. 36 (4):414-424. . Giri VN, Hegarty SE, Hyatt C, O'Leary E, Garcia J, Knudsen KE, et al. Germline genetic tests for hereditary prostate cancer in practice: Implications for genetic testing, precision therapy and cascade tests. Prostate. 2019 Mar. 79 (4):333-339. . Nicolosi P, Ledet E, Yang S, Michalski S, Freschi B, O'Leary E, et al. Prevalence of Germlin Variants in Prostate Cancer and Implications for the current Genetic Test Guidelines. JAMA Oncol. 2019 Apr 1. 5 (4):523-528. Na R, Zheng SL, Xu J, Isaacs WB. Germline mutations in ATM and BRCA1/2 Distinguished risk for deadly and painless prostate cancer and are associated with the early age of death. Eur Urol. 2017 May. 71 (5):740-747. . Marshall CH, Sokolova AO, McNatty AL, Cheng HH, Eisenberger MA, Bryce AH, et al. Differential response to the treatment of olaparib among men with prostate cancer resistant to castration resistant BRCA1 or BRCA2 Versus ATM Mutations. Eur Urol. 2019 Oct. 76 (4):452-458. . Raymond VM, Mukherjee B, Wang F, Huang SC, Stoffel EM, Kastrinos F, et al. High risk of prostate cancer among men with Lynch syndrome. J Clin Oncol. 2013 Mar 25. Cao Y, Ma J. Body mass index, specific mortality of prostate cancer and biochemical recurrence: systematic review and metaanalysis. Cancer Prev Res (Phila). 2011 Apr. 4 (4):486-501. . Ma J, Li H, Giovannucci E, Mucci L, Qiu W, Nguyen PL, et al. Prediagnostic body mass index, peptide plasma concentration and prostate cancer specific mortality in men with prostate cancer: long-term survival analysis. Lancet Oncol. 2008 Nov. 9 (11):1039-47. Stevens VL, Jacobs EJ, Sun J, Gapstur SM. There is no association of adiponectin and c-peptide plasma levels with risk of aggressive prostate cancer in the Nutrition Cohort of the Cancer Prevention Study II. Epidemiol Cancer Biomarkers Prev. 2014 May. 23 (5):890-2. Pischon T, Boeing H, Weikert S, Allen N, Key T, ...Slimani N, et al. Body size and risk of prostate cancer in European prospective research on cancer and nutrition. Epidemiol Cancer Biomarkers Prev. 2008 Nov. 17 (11):3252-61. Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC. Height, body weight and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev. 1997 Aug. 6 (8):557-63. . Mucci LA, Wilson KM, Giovannucci EL. Epidemiology of prostate cancer. Loda M, Mucci LA, Mittelstadt ML, Van Hemelrijck M, Cotter MB. Pathology and Epidemiology of Cancer. Springer International Publishing; 2017. 107-125. Klein EA, Thompson IM Jr, Tangen CM, Crowley JJ, Lucia MS, Goodman PJ, et al. Vitamin E and the risk of prostate cancer: the trial for the prevention of selenium and vitamin E cancer (SELECT). JAMA. 2011 Oct 12. 306 (14):1549-56. Gaziano JM, Glynn RJ, Christen WG, Kurth T, Belanger C, MacFadyen J, et al. Vitamins E and C in the prevention of prostate and total cancer in men: the health study of doctors II randomized controlled trial. JAMA. 2009 Jan 7. 301 (1):52-62. Eggener SE, Scardino PT, Walsh PC, Han M, et al. Predict the specific mortality of prostate cancer 15 years after radical prostatectomy. J Urol. 2011 Mar. 185(3):869-75. Cooperberg MR, Broering JM, Carroll PR. Evaluation of the risk of metastases and mortality at the time of diagnosis. J Natl Cancer Inst. 2009 Jun 16. 101(12):878-87. . .Kenfield SA, Stampfer MJ, Chan JM, Giovannucci E. Smoking and survival and recurrence of prostate cancer. JAMA. 2011 Jun 22. 305(24):2548-55. . .Joshu CE, Mondul AM, Meinhold CL, Humphreys EB, Han M, Walsh PC, et al. Recidive of smoking cigarettes and prostate cancer after prostatectomy. J Natl Cancer Inst. 2011 May 18. 103(10):835-8. Li WQ, Qureshi AA, Ma J, Goldstein AM, Giovannucci EL, Stampfer MJ, et al. Personal history of prostate cancer and increased risk of melanoma incidents in the United States. J Clin Oncol. 2013 Nov 4. Lamy PJ, Allory Y, Gauchez AS, Asselain B, Beuzeboc P, Cremoux P, et al. Biomarkers for localized management of prostate cancer: a systematic review. Eur Urol Focus. 2018 Dec. 4 (6):790-803. . Prostate cancer. National Comprehensive Cancer Network. Available in . Version 3.2020 — November 17, 2020; Accessed: December 29, 2020. Naji L, Randhawa H, Sohani Z, Dennis B, Lautenbach D, Kavanagh O, et al. Rectal Digital Exam for Detection of Prostate Cancer in Primary Care: A Systemic Test and Metaanalysis. Ann Fam Med. 2018 Mar. 16 (2):149-154. Hu JC, Nguyen P, Mao J, Halpern J, Shoag J, Wright JD, et al. Increase in distant metastases of prostate cancer in diagnosis in the United States. JAMA Oncol. 2017 May 1. 3 (5):705-707. . Pinsky PF, Prorok PC, Yu K, Kramer BS, Black A, Gohagan JK, et al. Extended mortality results for the diagnosis of prostate cancer in the PLCO trial with an average follow-up of 15 years. Cancer. 2017 Feb 15. 123 (4):592-599. . Schröder FH, Hugosson J, Roobol MJ, ....Auvinen A, ERSPC Investigators. Prostate cancer and screening mortality: results of the European random screening study for prostate cancer (ERSPC) to 13 years of follow-up. Lancet. 2014 Dec 6. 384 (9959):2027-35. Arnsrud Godtman R, Holmberg E, Lilja H, Stranne J, Hugosson J. Opportunistic tests against detection of prostate-specific organized antigens: result after 18 years in Göteborg randomized prostate cancer screening. Eur Urol. 2015 Sep. 68 (3):354-60. . Roobol MJ, Kerkhof M, Schröder FH, Cuzick J, ...Hugosson J, Auvinen A. Reduction of prostate cancer mortality from specific prostate antigen detection adjusted for non-assistance and contamination in the European random screening study for prostate cancer (ERSPC). Eur Urol. 2009 Oct. 56 (4):584-91. . Tabár L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, et al. Two Swedish counties test: impact of mammography detection on breast cancer mortality for 3 decades. Radiology. 2011 Sep. 260 (3):658-63. Siu AL, U.S. Preventive Services Task Force. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016 Feb 16. 164 (4):279-96. Carlsson S, Vickers AJ, Roobol M, Eastham J, Scardino P, Lilja H, et al. Prostate Cancer Review: Facts, Statistics and Interpretation in response to the review of the United States Preventive Services Task Force. J Clin Oncol. 2012 Jul 20. 30 (21):2581-4. . Butler SS, Muralidhar V, Zhao SG, Sanford NN, Franco I, Fullerton ZH, et al. The incidence of prostate cancer at all stages, NCCN risk groups, and age before and after the recommendations of USPSTF grade D against the detection of specific prostate antigen in 2012. Cancer. 2020 Feb 15. 126 (4):717-724. . Wilt TJ, Vo TN, Langsetmo L, Dahm P, Wheeler T, Aronson WJ, et al. Radical prostatectomy or observation for prostate cancer clinically located: Extended follow-up to Prostate Cancer Intervention Versus Observation Test (PIVOT). Eur Urol. 2020 Jun. 77 (6):713-724. U.S. Preventive Services Task Force, Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB, et al. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018 May 8. 319 (18):1901-1913. . Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, et al. Detection Cancer in the United States, 2019: A review of the current guidelines of the American Cancer Society and the current problems in cancer detection. CA Cancer J Clin. 2019 May. 69 (3):184-210. . Mottet N, Bellmunt J, ...Schoots IG, Wiegel T, Cornford P. EAU-ESTRO-SIOG Guidelines on prostate cancer. Part 1: Projection, Diagnosis and Local Treatment with Curative Intent. Eur Urol. 2017 Apr. 71 (4):618-629. . Carroll PR, Parsons JK, Andriole G, ...Dra cabeza, Ho M, Red Nacional de cáncer integral. Early detection of prostate cancer, version 1.2014. Featured updates of the NCCN Guidelines. J Natl Compr Canc Netw. 2014 Sep 12 (9):1211-9; maybe 1219. . Daskivich TJ, Fan KH, Koyama T, Albertsen PC, Goodman M, Hamilton AS, et al. Effect of age, tumor risk, and comorbidity on competing risks for survival in an American population cohort of men with prostate cancer. Ann Intern Med. 2013 May 21. 158 (10):709-17. . American Cancer Society Recommendations for the early detection of prostate cancer. American Cancer Society. Available on August 1, 2019; Access: May 22, 2020.Bul M, van Leeuwen PJ, Zhu X, Schröder FH, Roobol MJ. The incidence of prostate cancer and the specific survival of men with a specific initial prostate antigen less than 3.0 ng/ml participating in ERSPC Rotterdam. Eur Urol. 2011 Apr 59(4):498-505. . Bul M, van Leeuwen PJ, Zhu X, Schröder FH, Roobol MJ. The incidence of prostate cancer and the specific survival of men with a specific initial prostate antigen less than 3.0 ng/ml participating in ERSPC Rotterdam. Eur Urol. 2011 Apr 59(4):498-505. . Shao YH, Albertsen PC, Roberts CB, Lin Y, Mehta AR, Stein MN, et al. Risk profiles and treatment patterns among men diagnosed as prostate cancer and a specific prostate antigen level below 4.0 ng/ml. Arch Intern Med. 2010 Jul 26. 170(14):1256-61. . Preston MA, Batista JL, Wilson KM, Carlsson SV, Gerke T, Sjoberg DD, et al. Prostatic-specific antigen levels in average life predict lethal prostate cancer. J Clin Oncol. 2016 Jun 13. . National Network of Comprehensive Cancer. Early detection of prostate cancer. National Comprehensive Cancer Network. Available in . Version 2.2019 — May 31, 2019; Accessed: May 22, 2020. Vickers AJ, Till C, Tangen CM, Lilja H, Thompson IM. Empirical evaluation of guidelines on prostate-specific antigen speed in screening prostate cancer. J Natl Cancer Inst. 2011 Mar 16. 103(6):462-9. Mohammed W, Davis NF, Elamin S, Ahern P, Brady CM, Sweeney P. Six nuclei in front of prostate biopsy of twelve nuclei: a retrospective study that compares accuracy, oncological results and safety. Go J Med Sci. 2016 Feb. 185 (1):219-23. . Bjurlin MA, Carter HB, Schellhammer P, Cookson MS, Gomella LG, Troyer D, et al. Optimization of initial prostate biopsy in clinical practice: sampling, labeling and processing specimens. J Urol. 2013 Jun. 189 (6):2039-46. Borghesi M, Ahmed H, Nam R, Schaeffer E, Schiavina R, Taneja S, et al. Complications After systemic prostate biopsy, random and image-guided. Eur Urol. 2017 Mar. 71 (3):353-365. . Stefanova V, Buckley R, Flax S, Spevack L, Hajek D, Tunis A, et al. Transperin prostate biopsies using local anesthesia: Experience with 1,287 patients. Prostate cancer screening rate, complications and patient tolerance. J Urol. 2019 Jun. 201 (6):1121-1126. . Pepe P, Aragona F. Morbidity after transperineal prostate biopsy in 3000 patients under 12 vs 18 vs over 24 needle nuclei. Urology. 2013 Jun. 81 (6):1142-6. . Xue J, Qin Z, Cai H, Zhang C, Li X, Xu W, et al. Comparison between transrectal and transperin prostate biopsy for prostate cancer detection: metaanalysis analysis and sequential test analysis. Oncotarget. 2017 Apr 4. 8 (14):23322-23336. . Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. Image of pI-RADS - Information and Data System: 2015, Version 2. Eur Urol. 2016 Jan. 69 (1):16-40. . Rosenkrantz AB, Verma S, Choyke P, Eberhardt SC, Eggener SE, Gaitonde K, et al. Prostate Magnetic Resonance Imaging and Magnetic Resonance Imaging Targeted Biopsy in Patients with a Prior Negative Biopsy: A consensus Statement by AUA and SAR. J Urol. 2016 Dec. 196 (6):1613-1618. . van der Leest M, Cornel E, Israël B,...Hulsbergen-van de Kaa C, Barentsz JO. Comparison of transrectal ultrasound biopsy Versus multiparametric Resonance of prostate Imaging with Subsequent Magnetic Resonance-guided Biopsy in Biopsy-naïve Men with Elevated Prostate-specific Antigeno: A multicenter clinical study of great perspective. Eur Urol. 2019 Apr. 75 (4):570-578. . Kasivisvanathan V, Rannikko AS, .... Moore CM, PRECISION Study Group Collaborators. Biopsy composed of magnetic or standard resonance for diagnosis of prostate cancer. N Engl J Med. 2018 May 10. 378 (19):1767-1777. . Hamoen EHJ, Hoeks CMA, Somford DM, van Oort IM, Vergunst H, Oddens JR, et al. Multiparametric Magnetic Resonance Value in series Images and Magnetic Resonance imaging Biopsies in men with low-risk prostate cancer in active surveillance after 1 Yr follow-up. Eur Urol Focus. 2019 May. 5 (3):407-415. . Tran GN, Leapman MS, Nguyen HG, Cowan JE, Shinohara K, Westphalen AC, et al. Imaging-Ultrasound Fusion Biopsy during active surveillance of prostate cancer. Eur Urol. 2017 Aug. 72 (2):275-281. . Nassiri N, Margolis DJ, Natarajan S, Sharma DS, Huang J, Dorey FJ, et al. Biopsy aimed at detecting Gleason's score increase during active surveillance for men with low-risk or intermediate prostate cancer. J Urol. 2017 Mar. 197 (3 Pt 1):632-639. . Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, et al. A contemporary prostate cancer classification system: an alternative validated to the Gleason score. Eur Urol. 2016 Mar. 69 (3):428-35. . Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, et al. The Consensus Conference of the International Society of Urological Pathology (ISUP) on the Gleason Degree of Prostatic Carcinoma: Definition of Grade Patterns and Proposal for a New Grade System. Am J Surg Pathol. 2016 Feb. 40 (2):244-52. . Buyyounouski MK, Choyke PL, McKenney JK, Sartor O, Sandler HM, Amin MB, et al. Prostate Cancer - Important Changes in the American Joint Committee on Cancer 8th edition Cancer Staging Manual. CA Cancer J Clin. 2017 May 6. 67 (3):245-253. . Poyet C, Nieboer D, Bhindi B, Kulkarni GS, Wiederkehr C, Wettstein MS, et al. Prediction of the risk of prostate cancer using the new versions of the European random study for the treatment of prostate cancer (ERSPC) and risk calculators for the prevention of prostate cancer (PCPT): independent validation and comparison in a contemporary European cohort. BJU Int. 2016 Mar. 117 (3):401-8. . Rowe SP, Gorin MA, Allaf ME, Pienta KJ, Tran PT, Pomper MG, et al. PET Image of the prostate-specific membrane antigen in prostate cancer: current state of art and future challenges. Prostate Cancer Prostatic Dis. 2016 Sep. 19 (3):223-30. . Mulcahy N. Updated to Predict the Severity of Prostate Cancer. Available in . Access: January 15, 2013. Eifler JB, Feng Z, Lin BM, Partin MT, Humphreys EB, Han M, et al. Updated nomogram for prostate cancer staging (Participation fees) based in 2006 to 2011. BJU Int. 2013 Jan. 111(1):22-9. Cooperberg MR, Broering JM, Carroll PR. Evaluation of the risk of metastases and mortality at the time of diagnosis. J Natl Cancer Inst. 2009 Jun 16. 101(12):878-87. . Lowry F. Reverified prostate cancer risk calculator now online. Medscape Medical News. 8 August 2014. Crawford ED, Blumenstein BA. Proposed substations for metastatic prostate cancer. Urology. 1997 Dec. 50(6):1027-8. . [Guideline] Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, et al. Clinically located prostate cancer: AUA/ASTRO/SUO Direct. Part II: Recommended approaches and details of specific care options. J Urol. 2018 Apr. 199 (4):990-997. . .PDQ Adults treatment editorial board. Treatment of prostate cancer (PDQ®). National Cancer Institute. Available in . July 22, 2020; Access: September 14, 2020.EAU Virtual: EUPROMS Study investigates the effect of treatment of prostate cancer on quality of life. ASCO Post. Available on July 20, 2020; Access: July 23, 2020.Wilt TJ, Jones KM, Barry MJ, Andriole GL, Culkin D, Wheeler T, et al. Prostatectomy Tracking versus Premature Prostate Cancer Observation. N Engl J Med. 2017 Jul 13. 377 (2):132-142. Froehner M, Koch R, Hübler M, Renner T, Borkowetz A, Zastrow S, et al. Just Iversen P, Madsen PO, Corle DK. Radical prostatectomy versus expectant treatment for early prostate carcinoma. Twenty-three years of follow-up to a possible randomized study. Scand J Urol Nephrol Suppl. 1995. 172:65-72. Bill-Axelson A, Holmberg L, Garmo H, Taari K, Busch C, Nordling S, et al. Radical prostatectomy or vigilant expectation in prostate cancer - 29 years of follow-up. N Engl J Med. 2018 Dec 13. 379 (24):2319-2329. Bruinsma SM, Bangma CH, Carroll PR, Leapman MS, Rannikko A, Petrides N, et al. Active surveillance for prostate cancer: narrative review of clinical guidelines. Nat Rev Urol. 2016 Mar. 13 (3):151-67. Litwin MS, Tan HJ. Diagnosis and treatment of prostate cancer: a review. JAMA. 2017 Jun 27. 317 (24):2532-2542. . Hamdy FC, Donovan JL, Lane JA, Mason M, ...Neal DE, ProtecT Study Group. Results 10 years after Monitoring, Surgery, or Radiation therapy for localized prostate cancer. N Engl J Med. 2016 Oct 13. 375 (15):1415-1424. Chen RC. Radiation therapy for prostate cancer: An evolving treatment modality. Urol Oncol. 2019 Sep. 37 (9):579-581. . Brooks NA, Boland RS, Strigenz ME, Mott SL, Brown JA. Nongenitourinary compositions associated with laparoscopic and radical retropubia prostatectomy assisted by robot: Unique institutional assessment of 1,100 patients over 11 years of age. Urol Oncol. 2018 Nov. 36 (11):501.e9-501.e13. Spector BL, Brooks NA, Strigenz ME, Brown JA. Bladder neck contract Following the Radical Laparoscopic Prostatectomy Retropubic versus Robotic-Assisted. Curr Urol. 2017 Aug. 10 (3):145-149. Menon M, Dalela D, Jamil M, Diaz M, Tallman C, Abdollah F, et al. Functional recovery, oncological results and postoperative complications after radical prostatectomy consisting of robots: a evidence-based analysis that compares Retzius' wiring and standard approaches. J Urol. 2018 May. 199 (5):1210-1217. Geinitz H, Thamm R, Keller M, Astner ST, Heinrich C, et al. Longitudinal study of intestinal symptoms and fecal continence in patients with radiation therapy formed for prostate cancer. Int J Radiat Oncol Biol Phys. 2011 Apr 1. 79(5):1373-80. Margel D, Baniel J, Wasserberg N, Bar-Chana M, Yossepowitch O. Radiation therapy for prostate cancer increases the risk of later rectangles cancer. Ann Surg. 2011 Dec. 254(6):947-50. . Nihei K, Ogino T, Onozawa M, Murayama S, Fuji H, Murakami M, et al. Multi-institutional Phase II study of proton beam therapy for prostate cancer confined by organs focused on the incidence of late rectal toxicities. Int J Radiat Oncol Biol Phys. 2011 Oct 1. 81(2):390-6. . Wallis CJ, Mahar AL, Choo R, Herschorn S, Kodama RT, Shah PS, et al. Second malignities after radiation therapy for prostate cancer: systematic review and meta-analysis. BMJ. 2016 Mar 2. 352:i851. . .Walsh PC. Anatomical radical prostatectomy: evolution of the surgical technique. J Urol. 1998 Dec. 160 (6 Pt 2):2418-24. Sriprasad S, Feneley MR, Thompson PM. History of the treatment of prostate cancer. Surg Oncol. 2009 Sep. 18 (3):185-91. . van Poppel H, Everaerts W, Tosco L, Joniau S. Open and robotic radical prostatectomy. Asian J Urol. 2019 Apr. 6 (2):125-128. . Lowrance WT, Eastham JA, Savage C, Maschino AC, Laudone VP, Dechet CB, et al. Contemporary patterns of open and robotic radical prostatectomy among urologists in the United States. J Urol. 2012 Jun. 187 (6):2087-92. . Oberlin DT, Flum AS, Lai JD, Meeks JJ. The effect of minimally invasive prostatectomy on the patterns of practice of American urologists. Urol Oncol. 2016 Jun. 34 (6):255.e1-5. McAlpine K, Forster AJ, Breau RH, McIsaac D, Tufts J, Mallick R, et al. Robotic surgery improves transfusion rate and perioperative results using a wide implementation process and multiple surgeon learning curves. Can Urol Assoc J. 2019 Jun. 13 (6):184-189. . Preisser F, Busto Martin L, Pompe RS, Heinze A, Haese A, Graefen M, et al. Effect of the bladder neck spacing to laparoscopic prostatectomy assisted by robot in postoperative continence rates and biochemical recurrence. Urol Oncol. 2020 Jan. 38 (1).e11-1.e16. . Sooriakumaran P, Pini G, Nyberg T, Derogar M, Carlsson S, Stranne J, et al. Erectile function and oncological results after radical prostatectomy with the help of Robot and Retropubic: Results of the open test of LAParoscópica Robot prostatectomy. Eur Urol. 2018 Apr. 73 (4):618-627. . Basiri A, of the Rosette JJ, Tabatabaei S, Woo HH, Laguna MP, Shemshaki H. Comparison of radical retropubia, laparoscopic and robotic prostatectomy: who is the winner? World J Urol. 2018 Apr. 36 (4):609-621. . [Guideline] Rosenthal SA, Bittner NH, Beyer DC, Demanes DJ, et al. American Society for Radiation Oncology (ASTRO) and American College of Radiology (ACR) Practice Guide for Permanent Transperinary Brachytherapy of Prostate Cancer. Int J Radiat Oncol Biol Phys. 2011 Feb 1. 79(2):335-41. D'Amico AV, Chen MH, Renshaw AA, Loffredo M, Kantoff PW. Androgen Repression and Radiation vs only for prostate cancer: a randomized trial. JAMA. 2008 Jan 23. 299(3):289-95. Jones CU, Hunt D, McGowan DG, Amin MB et al. Radiation therapy and short-term androgen deprivation for localized prostate cancer. N Engl J Med. 2011 Jul 14. 365(2):107-18. . Pisansky TM, Hunt D, Gomella LG, Amin MB, Balogh AG, Chinn DM, et al. Duration of androgen suppression before radiation therapy for local prostate cancer: radiation therapy group oncology randomized clinical trial 9910. J Clin Oncol. 2015 Feb 1. 33 (4):332-9. . Clinical localized prostate cancer therapies: updating a 2008 systemic test. AHRQ. Available on December 16, 2014; Access: September 14, 2020. Bolla M, et al; European Organisation for Research and Treatment of Cancer, Radiation Oncology and Genito-Urinary Groups. Postoperative radiation therapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomized controlled trial (EORTC essay 22911). Lancet, 2012 Dec 8, 380 (9858):2018-27. Thompson IM Jr, Tangen CM, Paradelo J, Lucia MS, Miller G, Troyer D, et al. Adjuvant radiation therapy for advanced pathologically prostate cancer: a randomized clinical trial. JAMA. 2006 Nov 15. 296 (19):2329-35. Wiegel T, Bartkowiak D, Bottke D, Bronner C, Steiner U, Siegmann A, et al. Adjuvant radiation therapy versus waiting and looking after radical prostatectomy: 10-year follow-up to the ARO 96-02/AUO AP 09/95 trial. Eur Urol. 2014 Aug. 66 (2):243-50. Hackman G, Taari K, Tammela TL, ...Hemminki A, FinnProstate Group. Random test of adjuvant radiation therapy after radical prostatectomy Versus Radical prostatectomy Only in prostate cancer Patients with positive margins or Extracapsular extension. Eur Urol. 2019 Nov. 76 (5):586-595. . Thompson IM, Valicenti RK, Albertsen P, Davis BJ, Goldenberg SL, Hahn C, et al. Adjuvant radiation therapy and rescue after prostatectomy: AUA/ASTRO Guideline. J Urol. 2013 Aug. 190 (2):441-9. . Shah TT, Peters M, Arya M, Ahmed HU. Respond to Zhipeng Mai's letter to the Editor re: Taimur T. Shah, Max Peters, David Eldred-Evans, et al. Short-term results of Primary Focal Criotherapy to treat non-target clinically significant clinically significant prostate cancer of a Multicenter Prospective Registry. Eur Urol 2019;76:98-105. Eur Urol. 2019 Sep. 76 (3):e63-e64. . Noweski A, Roosen A, Lebdai S, Barret E, Emberton M, Benzaghou F, et al. Medium-term follow-up to Vascular Photodynamic Therapy of Prostate Cancer located using TOOKAD Soluble WST-11 (Phase II Trials). Eur Urol Focus. 2019 Nov. 5 (6):1022-1028. . Wang L, Yang H, Li B. Photodynamic therapy for prostate cancer: systematic review and metaanalysis. Prostate Int. 2019 Sep. 7 (3):83-90. . Kimura M, Mouraviev V, Tsivian M, Mayes JM, Satoh T, Polascik TJ. Current recovery methods for recurrent prostate cancer after the failure of primary radiation therapy. BJU Int. 2010 Jan. 105 (2):191-201. Bahn D, by Castro Abreu AL, Gill IS, Hung AJ, Silverman P, Gross ME, et al. Focus Criotherapy for clinically unilateral and intermediated prostate cancer in 73 men with an average follow-up of 3.7 years. Eur Urol. 2012 Jul. 62(1):55-63. . Lowrance W, Breau R, Chou R, et al. Advanced prostate cancer: AUA/ASTRO/SUO Guideline. American Urological Association. Available in . 25 June 2020; Access: 22 July 2020. Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Test design and goals for prostate castration-resistant cancer: Updated working group recommendations on prostate cancer 3. J Clin Oncol. 2016 Apr 20. 34 (12):1402-18. . Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Risk of mortality specific to prostate cancer after biochemical recurrence after radical prostatectomy. JAMA. 2005 Jul 27. 294(4):433-9. . Fu AZ, Tsai HT, Haque R, Yood MU, Cassidy-Bushrow AE, Van Den Eeden SK, et al. Mortality and Androgen Deprivation Therapy as Salvage Treatment for Biochemical Recurrence after Primary Therapy for Clinically Localized Prostate Cancer. J Urol. 2017 Jun. 197 (6):1448-1454. . García-Albeniz X, Chan JM, Paciorek A, Logan RW, Kenfield SA, Cooperberg MR, et al. Immediately against the deferred initiation of androgen deprivation therapy in patients with prostate cancer relapsed only by PSA. An observational follow-up study. Eur J Cancer. 2015 May. 51 (7):817-24. . Crook JM, O'Callaghan CJ, Duncan G, Dearnaley DP, et al. Intermittent androgen Repression for the increase in PSA level after radiation therapy. N Engl J Med. 2012 Sep 6. 367(10):895-903. . .Maximum androgen block in advanced prostate cancer: an overview of the randomised trials. Prostate Cancer Trial Collaborative Group. Lancet. 2000 Apr 29. 355(9214):1491-8. Huggins C, Hodges CV. Prostatic cancer studies. Me. The effect of castration, estrogen and androgen injection in serum phosphates in metastatic carcinoma of the prostate. Cancer Res. 1941;1:293-7. Byar DP, Corle DK. Hormonal therapy for prostate cancer: results of studies of the Veterans Cooperative Urological Research Group. NCI Monogr. 1988. 165-70. . Crawford ED, Blumenstein BA, Goodman PJ, et al. Leuprolide with and without flutamine in advanced prostate cancer. Cancer. 1990 Sep 1. 66(5 Suppl):1039-44. . Immediate treatment against deferred for advanced prostatic cancer: initial results of the Medical Research Council trial. The Medical Research Council Prostate Cancer Working Party Investigators Group. Br J Urol. 1997 Feb. 79(2):235-46. Calais da Silva FE, Bono AV, Whelan P, Brausi M, et al. Intermittent androgen deprivation for locally advanced and metastatic prostate cancer: results of a randomized phase 3 study of the Sureuropeo Group. Eur Urol. 2009 Jun. 55(6):1269-77. Hussain M, Tangen CM, Berry DL, Higano CS, Crawford ED, Liu G, et al. Intermittent deprivation of androgen in prostate cancer. N Engl J Med. 2013 Apr 4. 368(14):1314-25. Fizazi K, Tran N, Fein L, et al; LATITUDE Investigators. Abiraterone more Prednisone in metastatic and chestnut-sensitive prostate cancer. N Engl J Med. 2017 Jul 27. 377 (4):352-360. . James ND, by Bono JS, Spears MR, et al, for STAMPEDE researchers. Abiraterone for Prostate Cancer Not previously treated with hormonal therapy. N Engl J Med. June 3, 2017. Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with first-line standard therapy in metastatic prostate cancer. N Engl J Med. 2019 Jul 11. 381 (2):121-131. . Armstrong AJ, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, Villers A, Azad A, et al. ARCHES: A random phase III study of androgen deprivation therapy with enzalutamide or placebo in men with hormone-sensitive metastatic prostate cancer. J Clin Oncol. 2019 Nov 10. 37 (32):2974-2986. Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M, et al. Chemohormonal therapy in sensitive hormone metastatic prostate cancer. N Engl J Med. 2015 Aug 5. 42 (9):863-6. . . James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of twelvetaxel, zoledronic acid, or both to first-line long-term hormonal therapy in prostate cancer (STAMPEDE): Survival results from an adaptive, multi-arm, multi-stage randomized controlled trial. Lancet. 2016 Mar 19. 387 (10024):1163-77. . Shore ND, Saad F, Cookson MS, et al, and the, HERO Study Investigators. Oral Relugolix for Androgen Therapy-Deprivation in advanced prostate cancer. N Engl J Med. 2020 Jun 4. 382 (23):2187-2196. Smith MR, Saad F, Coleman R, Shore N, Fizazi K, Tombal B, et al. Survival without denosumab and bone metastases in men with prostate cancer resistant to castration: results of a phase 3, randomized placebo-controlled trial. Lancet. 2012 Jan 7. 379 (9810):39-46. Bryce AH, Alumkal JJ, Armstrong A, Higano CS, Iversen P, Sternberg CN, et al. Radiographic progression with PSA non-insurrection in metastatic prostate cancer prostate: PREVAIL post hoc analysis. Prostate Cancer Prostatic Dis. 2017 Jun. 20 (2):221-227. . Qi WX, Shen Z, Yao Y. Docetaxel therapy with or without estramustine as frontline chemotherapy for prostate cancer resistant to castration: a metaanalysis of four randomized controlled trials. J Cancer Res Clin Oncol. 2011 Dec. 137(12):1785-90. . Petrylak DP, Tangen CM, Hussain MH, Lara PN Jr, Jones JA, Taplin ME, et al. Docetaxel and estramustine compared to mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004 Oct 7. 351 (15):1513-20. Tannock IF, by Wit R, Berry WR, Horti J, Pluzanska A, et al. Docetaxel more prednisone or mitoxantrone more prednisone for advanced prostate cancer. N Engl J Med. 2004 Oct 7. 351(15):1502-12. Berthold DR, Pond GR, Soban F, Wit R, Eisenberger M, Tannock IF. Docetaxel more prednisone or mitoxantrone more prednisone for advanced prostate cancer: updated survival in the TAX 327 study. J Clin Oncol. 2008 Jan 10. 26(2):242-5. Smith M, De Bono J, Sternberg C, Le Moulec S, Oudard S, et al. Phase III Cabozantinib study in metastatic castration-resistant prostate cancer previously treated: COMET-1. J Clin Oncol. 2016 Jul 11. Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for prostate cancer resistant to castration. N Engl J Med. 2010 Jul 29. 363 (5):411-22. .de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and greater survival in metastatic prostate cancer. N Engl J Med. 2011 May 26. 364(21):1995-2005. . .Fizazi K, Scher HI, Molina A, Logothetis CJ, Chi KN, et al. Abiraterone's acetate for the treatment of metastatic prostate cancer: final overall survival analysis of phase 3 randomized, double-blind placebo-controlled study. Lancet Oncol. 2012 Oct. 13(10):983-92. U.S. Food and Drug Administration FDA expands the use of Zytiga for late-stage prostate cancer. 10 December 2012. Available in . Access: December 17, 2012. Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012 Sep 27. 367(13):1187-97. . Shore ND, Chowdhury S, Villers A, Klotz L, Siemens DR, Phung D, et al. Effectiveness and safety of enzalutamide against bicalutamide for patients with metastatic prostate cancer (TERRAIN): a randomized, double-blind, phase 2. Lancet Oncol. 2016 Feb. 17 (2):153-63. Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, et al. Enzalutamide in men with non-target and castration-resistant prostate cancer. N Engl J Med. 2018 Jun 28. 378 (26):2465-2474. . de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP,et al. Prednisone plus colazitaxel or mitoxantrona for metastatic castration-resistant prostate cancer that progresses after the treatment of twelvetaxel: a randomized open label trial. Lancet. 2010 Oct 2. 376(9747):1147-54. Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, et al. Apalutamide treatment and survival without metastasis in prostate cancer. N Engl J Med. 2018 Feb 8. Fizazi K, et al. Darolutamide in non-target and castration-resistant prostate cancer. N Engl J Med. 2019 Mar 28. 380 (13):1235-1246. . . Abida W, Campbell D, Patnaik A, Sautois B, Shapiro J, Vogelzang NJ, et al. Preliminary results of the study TRITON2 of rucaparib in patients (pts) with DNA damage repair (DDR) poor prostate cancer resistant to metastatic castration (mCRPC): updated analysis. Ann Oncol 2019;30 (suppl 5):abst 846PD. .de Bono J, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Olaparib for prostate cancer resistant to metastatic castration. N Engl J Med. 2020 Apr 28. . Targeted therapy Accelerates the progress of advanced prostate cancer [ESMO 2019 Press release]. European Society for Medical Oncology. Available in . September 30, 2019; Access: December 19, 2019. Hussain M, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Survival with Olaparib in prostate cancer resistant to metastatic castration. N Engl J Med. 2020 Sep 20. Brooks M. FDA Grants Expanded Indication for Enzalutamide (Xtandi). Medscape Medical News. Available in . Access: September 14, 2014. Rusthoven CG, Jones BL, Flaig TW, Crawford ED, Koshy M, Sher DJ, et al. Better survival with prostate radiation in addition to androgen deprivation therapy for men with newly diagnosed metastatic prostate cancer. J Clin Oncol. 2016 Jun 20. . Roqué I Figuls M, Martinez-Zapata MJ, Scott-Brown M, Alonso-Coello P. Radioisotopes for metastatic bone pain. Cochrane Database Syst Rev. 2011 Jul 6. CD003347. Food and Drug Administration. The FDA approves new medication for advanced prostate cancer [press release]. 15 May 2013. Available in . Access: July 1, 2013. Chustecka Z. Xofigo (Radium-223) Approved for prostate cancer with bone metes. Medscape Medical News. Available in . Access: June 11, 2013. Brady D, Parker CC, O'Sullivan JM. Bone perforation radiopharmaceuticals including radio-223. Cancer J. 2013 Jan. 19(1):71-8. Hoskin P, Sartor O, O'Sullivan JM, Johannessen DC, Helle SI, Logue J, et al. Effectiveness and safety of dichloride radium-223 in patients with prostate cancer resistant to castration and symptomatic bone metastases, with or without previous use of twelvetaxel: a preset subgroup analysis of randomized, double-blind trial, phase 3 ALSYMPCA. Lancet Oncol. 2014 Nov. 15 (12):1397-406. . Smith MR, Saad F, Egerdie B, Sieber PR, Tammela TL, Ke C, et al. Sarcopenia during androgen deprivation therapy for prostate cancer. J Clin Oncol. 2012 Sep 10. 30(26):3271-6. . .FDA Drug safety communication: Update to the continuous safety review of GnRH agonists and notification to GnRH agonists manufacturers to add new safety information to the labeling of the highest risk of diabetes and certain cardiovascular diseases. U.S. Drug Administration Available on October 20, 2010; Access: February 16, 2018.Gillessen S, Templeton A, Marra G, Kuo YF, Valtorta E, Shahinian VB. Risk of colorectal cancer in men in long-term androgen deprivation therapy for prostate cancer. J Natl Cancer Inst. 2010 Dec 1. 102(23):1760-70. Morgans AK, Hancock ML, Barnette KG, Steiner MS, Morton RA, Smith MR. Racial differences in bone mineral density and fractures in men who receive androgen deprivation therapy for prostate cancer. J Urol. 2012 Mar. 187(3):889-93. . Mulcahy N. New Risk With ADT in Prostate Cancer: Kidney Injuries. Medscape Medical News. Available in . Access: July 23, 2013.Lapi F, Azoulay L, Niazi MT, Yin H, Benayoun S, Suissa S. Androgen deprivation therapy and risk of acute kidney injury in patients with prostate cancer. JAMA. 2013 Jul 17. 310(3):289-96. Boonen S, Reginster JY, Kaufman JM, Lippuner K, et al. Risk of fracture and zoledronic acid therapy in men with osteoporosis. N Engl J Med. 2012 Nov. 367(18):1714-23. . Smith MR, Egerdie B, Hernández Toriz N, Feldman R, et al. Denosumab in men who receive androgen deprivation therapy for prostate cancer. N Engl J Med. 2009 Aug 20. 361(8):745-55. . .Fizazi K, Carducci M, Smith M, Damião R, Brown J, etc. Denosumab versus zoledronic acid for the treatment of bone metastases in men with prostate cancer resistant to castration: a randomized and double-blind study. Lancet. 2011 Sea 5. 377(9768):813-22. . .[Guideline] Laidman J. New ACS Guide for PCPs Prostate Cancer Survivors Management. Medscape Medical News. 11 June 2014. [Guideline] Bankhead C. Prostate Ca Guidelines Center on Primary Care. MedPage Today. Jun 11 2014. .Abramowitz MC, Li T, Buyyounouski MK, Ross E, Uzzo RG, Pollack A, et al. The Phoenix definition of biochemical failure predicts overall survival in patients with prostate cancer. Cancer. 2008 Jan 1. 112(1):55-60. Dickinson L, Ahmed HU, Allen C, Barentsz JO, Carey B,et al. MRI images for the detection, location and characterization of prostate cancer: recommendations of a European consensus meeting. Eur Urol. 2011 Apr 59(4):477-94. . Gaziano JM, Glynn RJ, Christen WG, Kurth T, Belanger C, et al. Vitamins E and C in the prevention of prostate and total cancer in men: the health study of doctors II randomized controlled trial. JAMA. 2009 Jan 7. 301(1):52-62. . Lippman SM, Klein EA, Goodman PJ, Lucia MS, et al. Effect of selenium and vitamin E on the risk of prostate cancer and other cancers: the trial for the prevention of selenium and vitamin E cancer (SELEC). JAMA. 2009 Jan 7. 301(1):39-51. . Liu Y, Hu F, Li D, Wang F, Zhu L, Chen W, et al. Does physical activity reduce the risk of prostate cancer? A systematic review and meta-analysis. Eur Urol. 2011 Nov. 60(5):1029-44. Thompson IM, Goodman PJ, Tangen CM, Lucia MS, Miller GJ, Ford LG, et al. The influence of finasteride in the development of prostate cancer. N Engl J Med. 2003 Jul 17. 349(3):215-24. . Andriole GL, Bostwick DG, Brawley OW, Gomella LG, et al. Effect of dutsteride on the risk of prostate cancer. N Engl J Med. 2010 Apr 1. 362(13):1192-202. Thompson IM, Goodman PJ, Tangen CM, Lucia MS, Miller GJ, Ford LG, et al. The influence of finasteride in the development of prostate cancer. N Engl J Med. 2003 Jul 17. 349 (3):215-24. . Redman MW, Tangen CM, Goodman PJ, Lucia MS, Coltman CA Jr, Thompson IM. Finasteride does not increase the risk of high-grade prostate cancer: a prejudge-adjusted modeling approach. Cancer Prev Res (Phila). 2008 Aug. 1 (3):174-81. . Andriole GL, Bostwick D, Brawley OW, Gomella L, Marberger M, Montorsi F, et al. The effect of dutsteride on the usefulness of the prostate-specific antigen for the diagnosis of high-grade and clinically relevant prostate cancer in men with a previous negative biopsy: results of the REDUCE study. J Urol. 2011 Jan. 185 (1):126-31. . Kramer BS, Hagerty KL, Justman S, Somerfield MR, et al. Use of 5 alpha-reductase inhibitors for chemoprevention of prostate cancer: American Society of Clinical Oncology/American Urological Association 2008 Guide to Clinical Practices. J Clin Oncol. 2009 Mar 20. 27(9):1502-16. . .FDA Drug Safety Communication: 5-alpha reductasehibiors (5-ARIs) may increase the risk of a more severe form of prostate cancer. U.S. Drug Administration Available in . 9 June 2011; Access: 16 February 2018. Fleshner NE, Lucia MS, Egerdie B, Aaron L, Eure G, Nandy I, et al. Dutasteride in localized management of prostate cancer: randomized, double-blind, placebo-controlled trial. Lancet. 2012 Mar 24. 379(9821):1103-11. . [Guideline] Screening for Prostate Cancer: Current Recommendation. United States Preventive Services Task Force. May 2012. United States Preventive Services Task Force. Available on May 8, 2018; Accessed: May 22, 2020.[Guideline] Qaseem A, Barry MJ, Denberg TD, Owens DK, Shekelle P. Screening for Prostate Cancer: A Guidance Statement From the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2013 Apr 9. Parker C, Gillessen S, Heidenreich A, Horwich A, ESMO Guidelines Committee. Prostate cancer: ESMO Guidelines for clinical practice for diagnosis, treatment and follow-up. Ann Oncol. 2015 Sep. 26 Suppl 5:v69-77. .[Guideline] Carter HB, Albertsen PC, Barry MJ, Etzioni R, Freedland SJ, Greene KL, et al. Early detection of prostate cancer: AUA guide. American Urological Association. Available in . 2015; Accessed: February 16, 2018.[Guideline] Mottet N, Bellmunt J, Briers E, et al. EAU-ESTRO-SIOG GUIDELINES ON PROSTATE CANCER. European Association of Urology. Available in . March 2016; Access: 14 September 2020. Hayes JH, Ollendorf DA, Pearson SD, Barry MJ, et al. Active surveillance compared to initial treatment for men with low-risk prostate cancer: a decision analysis. JAMA. 2010 Dec 1. 304(21):2373-80. . .[Guideline] Chen RC, Rumble RB, Loblaw DA, Finelli A, Ehdaie B, Cooperberg MR, et al. Active surveillance for the management of localized prostate cancer ( Ontario Cancer Care Directive): American Society of Clinical Oncology Clinical Practices Orientation Practices. J Clin Oncol. 2016 Jun 20. 34 (18):2182-90. . .[Guideline] Basch E, Loblaw DA, Oliver TK, Carducci M, Chen RC, Frame JN, et al. Systemic therapy in men with metastatic castration-resistant prostate cancer: American Society of Clinical Oncology and Cancer Care Ontario clinic practiceline guide. J Clin Oncol. 2014 Oct 20. 32 (30):3436-48. Trabulsi EJ, Rumble RB, Jadvar H, et al. Optimal strategies for advanced prostate cancer: ASCO Guideline. J Clin Oncol. 2020 Jan 15. JCO1902757. . DeCastro GJ, Jayram G, Razmaria A, Shalhav A, Zagaja GP. Functional results in African Americans after radical prostatectomy assisted by robot. J Endourol. 2012 Aug. 26(8):1013-9. Smith MR, Saad F, et al. Survival without denosumab and bone metastases in men with prostate cancer resistant to castration: results of a phase 3, randomized placebo-controlled trial. Lancet. 2012 Jan 7. 379(9810):39-46. Schumacher MC, Burkhard FC, Thalmann GN, Fleischmann A, Studer UE. Good result for patients with few lymph node metastases after radical retropubia prostatectomy. Eur Urol. 2008 Aug. 54(2):344-52. Messing EM, Manola J, Sarosdy M, Wilding G, Crawford ED, Trump D. Immediate hormone therapy compared to observation after radical prostatectomy and pelvic lymphodenectomy in men with positive node prostate cancer. N Engl J Med. 1999 Dec 9. 341(24):1781-8. . Bolla M, de Reijke TM, Van Tienhoven G, Van den Bergh AC, et al. Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med. 2009 Jun 11. 360(24):2516-27. . Bria E, Cuppone F, Giannarelli D, Milella M, et al. Is hormonal treatment added to radiation therapy improving the outcome of locally advanced prostate cancer?: randomized test metaanalysis. Cancer. 2009 Aug 1. 115(15):3446-56. . Mulcahy N. Radiotherapy Plus ADT Benefit Confirmed in high-risk prostate cancer. Medscape [serial online]. Available in . Access: February 3, 2014. Ewing CM, Ray AM, Lange EM, Zuhlke KA, Robbins CM, et al. Germline mutations in HOXB13 and risk of prostate cancer. N Engl J Med. 2012 Jan 12. 366(2):141-9. Fowler JE Jr, Sanders J, Bigler SA, Rigdon J, Kilambi NK, Land SA. Detection of antigen and cancer in white and black men with specific prostate antigen total 2.5 to 9.9 ng./ml. J Urol. 2000 May. 163(5):1467-70. Scavonetto F, Yeoh TY, Umbreit EC, et al. Association between neurological analgesia, progression of cancer and mortality after radical prostatectomy: a large and retrospective cohort study. Br J Anaesth. 2013 Dec 16. Markert EK, Mizuno H, Vazquez A, Levine AJ. Molecular classification of prostate cancer by curated expression firms. Proc Natl Acad Sci U S A. 2011 Dec 27. 108(52):21276-81. Ilic D, Djulbegovic M, Jung JH, Hwang EC, Zhou Q, Cleves A, et al. Prostate cancer screening test with prostate-specific antigen: systematic review and meta-analysis. BMJ. 2018 Sep 5. 362:k3519. . . American Urological Association. Recommendations of the AU Disputes Group on Prostate Cancer Analysis. Available in . May 21, 2012; Access: August 6, 2019. Andriole GL, Crawford ED, Grubb RL 3rd, Buys SS, et al. Mortality is the result of a randomized prostate cancer screening. N Engl J Med. 2009 Mar 26. 360(13):1310-9. . .Schröder FH, Hugosson J, Roobol MJ, Tammela TL, et al. Prostate cancer screening and mortality in a randomized European study. N Engl J Med. 2009 Mar 26. 360(13):1320-8. . Page EC, Bancroft EK, Brook MN, et al. Interim results of the IMPACT study: Evidence for the detection of prostate-specific antigens in BRCA2 mutation carriers. Eur Urol. 2019 Sep 16. . . Ahmed HU, Bosaily AE-S, Brown LC, et al; PROMIS study group. Diagnostic precision of multiparametric MRI and TRUS biopsy in prostate cancer (PROMIS): a peer-to-peer validator confirming study. Lancet. 19 January 2017. Cornelis F, Rigou G, Le Bras Y, et al. Transrectal prostate biopsy led by the United States in real time: diagnostic precision in men with previously negative biopsy results and positive results of the MR. Radiology. 2013 Oct. 269(1):159-66. Stewart GD, Van Neste L, Delvenne P, Delrée P, Delga A, McNeill SA, et al. Clinical use of an epigenetic trial to detect occult prostate cancer in histopathologically negative biopsies: results of the MATLOC study. J Urol. 2013 Mar. 189 (3):1110-6. . National Cancer Institute. Prostate Cancer Screening (PDQ®). Available on April 22, 2020; Access: May 22, 2020. Rosario DJ, Lane JA, Metcalfe C, Donovan JL, Double A, et al. Short-term results of prostate biopsy in men tested for prostate-specific antigen cancer: prospective evaluation within the ProtecT study. BMJ. 2012 Jan 9. 344:d7894. . . Eiber M, Rauscher I, Souvatzoglou M, Maurer T, Schwaiger M, Holzapfel K, et al. Prospective comparison of the head to head of 11C-choline-PET/MR and 11C-choline-PET/CT for re-installing recurrent biochemical prostate cancer. Eur J Nucl Med Mol Imaging. 2017 Dec. 44 (13):2179-2188. [Guideline] Expert Panel on Urologic Images: Coakley FV, Oto A, Alexander LF, Allen BC, Davis BJ, et al. ACR Appropriateness Criteria® Prostate Cancer-Pretreatment Detection, Surveillance and Staging. J Am Coll Radiol. 2017 May. 14 (5S):S245-S257. . Ellis RJ, Kaminsky DA, Zhou EH, Fu P, Chen WD, Brelin A, et al. 10-year results: the clinical utility of issuing individual photons computed tomography/computed tomography capromab pendetide (Prostascint) in a cohort diagnosed with local prostate cancer. Int J Radiat Oncol Biol Phys. 2011 Sep 1. 81(1):29-34. Haese A, Epstein JI, Huland H, Partin AW. Validation of a pathological algorithm based on biopsy to predict lymph node metastases in patients with prostate carcinoma clinically located. Cancer. 2002 Sep 1. 95(5):1016-21. . Lu-Yao GL, Albertsen PC, Moore DF, Shih W, Lin Y, DiPaola RS, et al. 15-year survival results after primary androgen therapy and deprivation for localized prostate cancer. JAMA Intern Med. 2014 Jul 14. . Cantiello F, Russo GI, Kaufmann S, Cacciamani G, Crocerossa F, Ferro M, et al. Function of multiparametric MRI for patients under active surveillance for prostate cancer: systematic review with diagnostic metaanalysis. Prostate Cancer Prostatic Dis. 2019 May. 22 (2):206-220. . NC leaves, Goldin GH, Meyer AM, Wu Y, Chang Y, et al. Radiation therapy modified by intensity, proton therapy or conformal radiation therapy and disease control in local prostate cancer. JAMA. 2012 Apr 18. 307(15):1611-20. Briganti A, Wiegel T, Joniau S, Cozzarini C, Bianchi M, et al. Early rescue radiation therapy does not compromise cancer control in patients with pT3N0 cancer after radical prostatectomy: results of a multi-institutional analysis controlled by the party. Eur Urol. 2012 Sep. 62(3):472-87. Mottet N, Bellmunt J, Bolla M, Joniau S, Mason M, et al. AUE guidelines on prostate cancer. Part II: Treatment of advanced prostate cancer, relapsed and resistant to castration. Eur Urol. 2011 Rev. 59(4):572-83. . de Vrij J, Willemsen RA, Lindholm L, Hoeben RC, et al. vectors of Adenovirus origin for the genetic therapy of prostate cancer. Hum Gene Ther. 2010 Jul. 21(7):795-805. . Hofman MS, Violet J, Hicks RJ, Ferdinandus J, Thang SP, Akhurst T, et al. [177Lu]-PSMA-617 treatment of radionuclides in patients with metastatic castration-resistant prostate cancer (LPSMA test): a single-center study, one arm, phase 2. Lancet Oncol. 2018 Jun. 19 (6):825-833. McBean R, O'Kane B, Parsons R, Wong D. Lu177-PSMA therapy for men with advanced prostate cancer: Initial 18-month experience in a single Australian tertiary institution. J Med Imaging Radiat Oncol. 2019 Apr 25. Huggins C, Hodges CV. Prostatic cancer studies. Me. The effect of castration, estrogen and androgen injection in serum phosphates in metastatic carcinoma of the prostate. Cancer Res. 1941;1:293-7. [Guideline] Cookson MS, Roth BJ, Dahm P, et al. Castration-resistant prostate cancer: AU Guide. American Urological Association. Available in . Published 2013; Amended 2018; Accessed: December 29, 2020. Kishan AU, Cook RR, Ciezki JP, ... King CR. Radical prostatectomy, External Beam Radiation therapy or external beam radiation therapy with brachytherapy outbreaks and disease and mortality progression in patients with prostate cancer 9-10. JAMA. 2018 Mar 6. 319 (9):896-905. . Lerner SP, Shen S. Pathological assessment and clinical significance of prostatic involvement by transitional cell carcinoma and prostate cancer. Urol Oncol. 2008 Sep-Oct. 26 (5):481-5. . Wood DP Jr, Montie JE, Pontes JE, VanderBrug Medendorp S, Levin HS. Transient cell carcinoma of the prostate in cytstoprostatectomy specimens eliminated for bladder cancer. J Urol. 1989 Feb. 141 (2):346-9. . Esrig D, Freeman JA, Elmajian DA, et al. Transit cell carcinoma that involves the prostate with a proposed staging classification for stroma invasion. J Urol. 1996 Sep. 156 (3):1071-6. Reese JH, Freiha FS, Gelb AB, Lum BL, Torti FM. Transient cell carcinoma of the prostate in patients undergoing radical cystoprostatectomy. J Urol. 1992 Jan. 147 (1):92-5. . Revelo MP, Cookson MS, Chang SS, Shook MF, Smith JA Jr, Shappell SB. Incidence and location of prostate and urotelial carcinoma in cystoprostatectomy prostates: implications for possible apical spacing surgery. J Urol. 2004 Feb. 171 (2 Pt 1):646-51. . Njinou Ngninkeu B, Lorge F, Moulin P, Jamart J, Van Cangh PJ. Transient cell carcinoma involving prostate: a retrospective clinical pathologic study of 76 cases. J Urol. 2003 Jan. 169 (1):149-52. . Shen SS, Lerner SP, Muezzinoglu B, Truong LD, Amiel G, Wheeler TM. Prostatic participation by transitional cell carcinoma in patients with bladder cancer and their prognostic significance. Hum Pathol. 2006 Jun. 37 (6):726-34. . Pettus JA, Al-Ahmadie H, Barocas DA, et al. Assessment of the risk of prostatic pathology in patients undergoing radical chestoprostatectomy. Eur Urol. 2008 Feb. 53 (2):370-5. . Komyakov BK, Sergeev AV, Fadeev VA, et al. [Concomitant oncopatological changes in the prostate of patients with urinary bladder cancer subjected to radical cystoprostateectomy] [Russian]. Urologiia. 2017 Sep. 42-5. Aharony S, Baniel J, Yossepowitch O. Positive urinary cytology without clinical confirmation: diagnostic implications and oncological results. BJU Int. 2011 Oct. 108 (8 pt 2):E179-83. . Cheville JC, Dundore PA, Bostwick DG, et al. Transient cell carcinoma of the prostate: clinical pathologic study of 50 cases. Cancer. 1998 Feb 15. 82 (4):703-7. . Kim HJ, Yoo JH. Cytokeratin 20/p53 dual immunocytochemicals to improve the diagnostic accuracy of liquid cytology in the detection of urotelial neoplasia: A retrospective study. Cytojournal. 2017. 14:27. . . Varinot J, Cussenot O, Roupret M, et al. HOXB13 is a sensitive and specific marker of prostate cells, useful for distinguishing between prostatic and urothelial carcinomas. Virchows Arch. 2013 Dec. 463 (6):803-9. . Olsen JR, Azeem W, Hellem MR, et al. Context regulatory patterns dependent on androgen receptor and androgen receptor genes. BMC cancer. 2016 Jul 4. 16:377. . .Chad R Tracy, Assistant Professor of MD, Department of Urology, University of Iowa, Roy J and Lucille A Carver College of Medicine Chad R Tracy, MD is a member of the following medical societies: , , Disclosure: Nothing to reveal. Nathan A Brooks, MD Resident Physician, Department of Urology, University of Iowa Hospitals and Clinics Nathan A Brooks, MD is a member of the following medical societies: Disclosure: Nothing to reveal. Mohammed Said, MD Fellow in Minimally Invasive Surgery and Endourology, Department of Urology, University of Iowa, Roy J and Lucille A Carver College of Medicine Disclosure: Nothing to reveal. Edward David Kim, MD, FACS Surgery Professor, Urology Division, University of Tennessee Medical Faculty; Consulting Cabinet, University of Tennessee Medical Center Edward David Kim, MD, FACS is a member of the following medical societies: , , , , , , Disclosure: Serve(d) as speaker or member of a speaker's office for: Endo. Tracey L Krupski, MD, Assistant Professor of MPH, Department of Urology, University of Virginia Medical School Tracey L Krupski, MD, MPH is a member of the following medical societies: , , , Disclosure: Nothing to reveal. Bagi RP Jana, MD, MBA, MHA, FACP Cancer Medicine Professor, MD Anderson Cancer Center; Medical Professor, Texas University Medical Branch at Galveston Bagi RP Jana, MD, MBA, MHA, FACP is a member of the following medical societies: , , , Disclosure: Nothing to reveal. Gerald W Chodak, MD , Editor, www.ProstateVideos.com; Medscape Urology, Experts and Viewpoints--Controversies in Urology; Director of Medical Content, Answers Media, LLC; Author, Winning the Battle Against Prostate Cancer Gerald W Chodak, MD is a member of the following medical societies: Disclosure: Nothing to reveal. Isamettin Andrew Aral, MD, MSc Attending Physician, Nassau Radiologic Group (Long Island Radiation Therapy); Assistant Professor of Radiational Oncology, New York State University Downstate College of MedicineIsamettin Andrew Aral, MD, MSc, is a member of the following medical societies: , , and Divulgation: Nothing to reveal. Hassan Aziz, MD Clinical Professor, Department of Radiation Oncology, Downstate Medical Center and Long Island College Hospital, State University of New York at DownstateHassan Aziz, MD is a member of the following medical societies: and Disclosure: Nothing to disclose. Michael Giasullo, MD Clinical Assistant Professor, Department of Urology, State University of New York Downstate Medical Center; Chief, Department of Surgery, Division of Urology, Lutheran Medical Center; Consulting Staff, Bay Ridge Urology Associates; Assistant Attending Physician, Department of Surgery, Urology Section, Methodist Hospital Michael Giasullo, MD is a member of the following medical societies: and Disclosure: Nothing to reveal. Leonard Gabriel Gomella, MD, FACS Professor Bernard W Godwin de Prostate Cancer Chairman, Department of Urology, Associate Director of Clinical Affairs, Kimmel Cancer Center, Jefferson Medical College of Thomas Jefferson UniversityLeonard Gabriel Gomella, MD,CS is a member of the following medical societies: , , , , , , , , Society of University Urologists, and MD Nicholas Karanikolas, MD Associate Professor, Department of Urology, SUNY Downstate College of Medicine; Director, Urologic Oncology, Staten Island University Hospital; Attending Physician, Department of Urology, Brooklyn Veterans Administration HospitalNicholas Karanikolas, MD is a member of the following medical societies: Disclosure: Nothing to reveal. Francisco Talavera, PharmD, PhD Associate Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-chief, Medscape Drug ReferenceDisclosure: Medscape Salary Employment Dan Theodorescu, MD, PhD Paul A Bunn Professor of Cancer Research, Professor of Surgery and Pharmacology, Director, University of Colorado Comprehensive Cancer Center Dan Theodorescu, MDromaDunder Stock
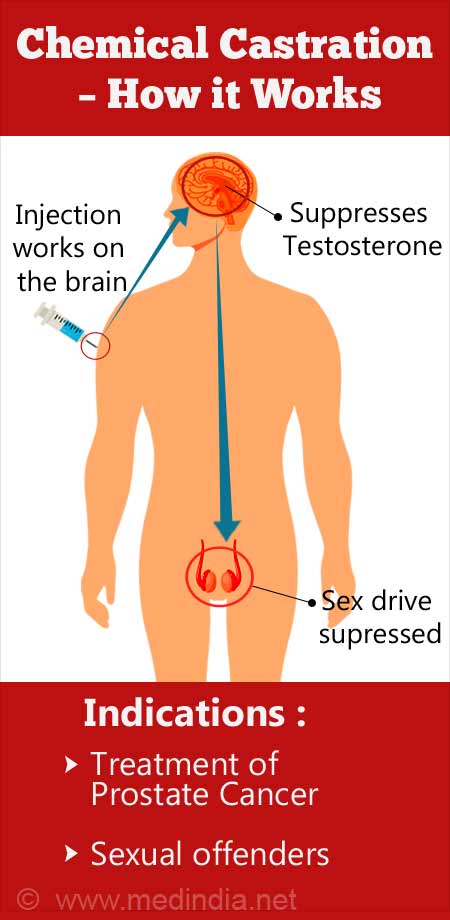
Chemical Castration - Medicine - Pros and Cons
Korea Herald
The side effects of castration in horses - and how osteopathic techniques can help

Chemical Castration - Medicine - Pros and Cons
Effects of Castration on the Life Expectancy of Contemporary Men - LessWrong
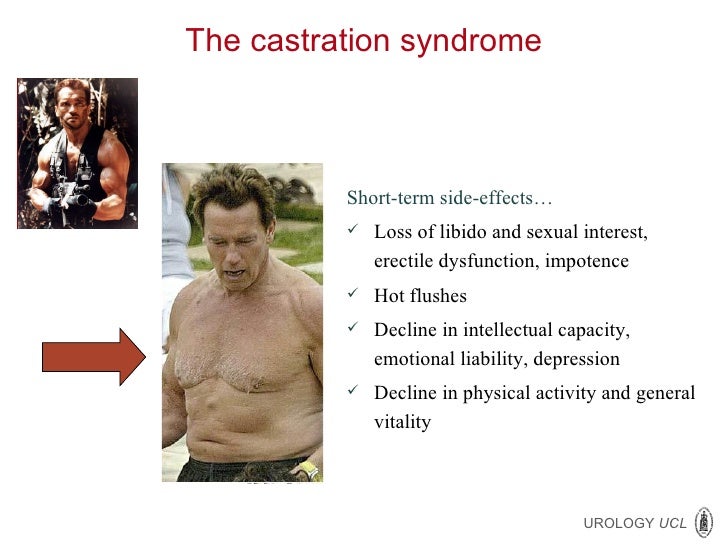
ECCLU 2011 - B. Tombal - Side-effects of anti-androgen therapy
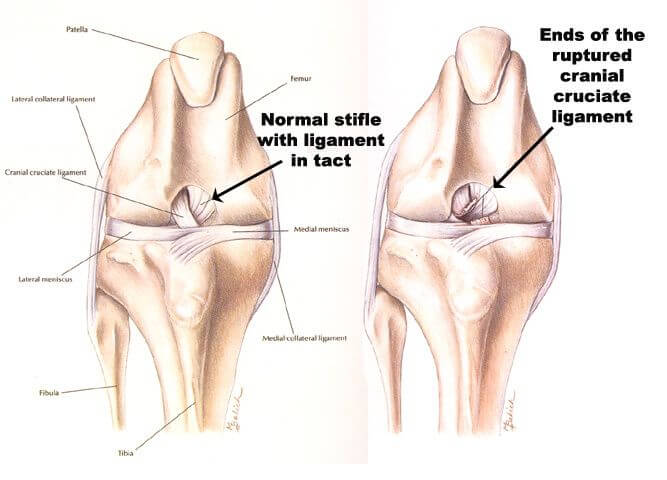
Dog Neutering: The Unspoken Risks Of Neutering | Dogs First

Why chemical castration of child rapists & molesters is a solution that ignores realities - The Economic Times

Castration - Wikipedia

What is chemical castration, how does it work and was it used on Michael Jackson?
COMMENTARY Long-Term Consequences of Castration in Men: Lessons from the Skoptzy and the Eunuchs of the Chinese and Ottoman Cour

Why chemical castration of child rapists & molesters is a solution that ignores realities - The Economic Times
Castration of Calves

Chemical Castration - Medicine - Pros and Cons
Castration of Calves
Dog Neutering: The Unspoken Risks Of Neutering | Dogs First
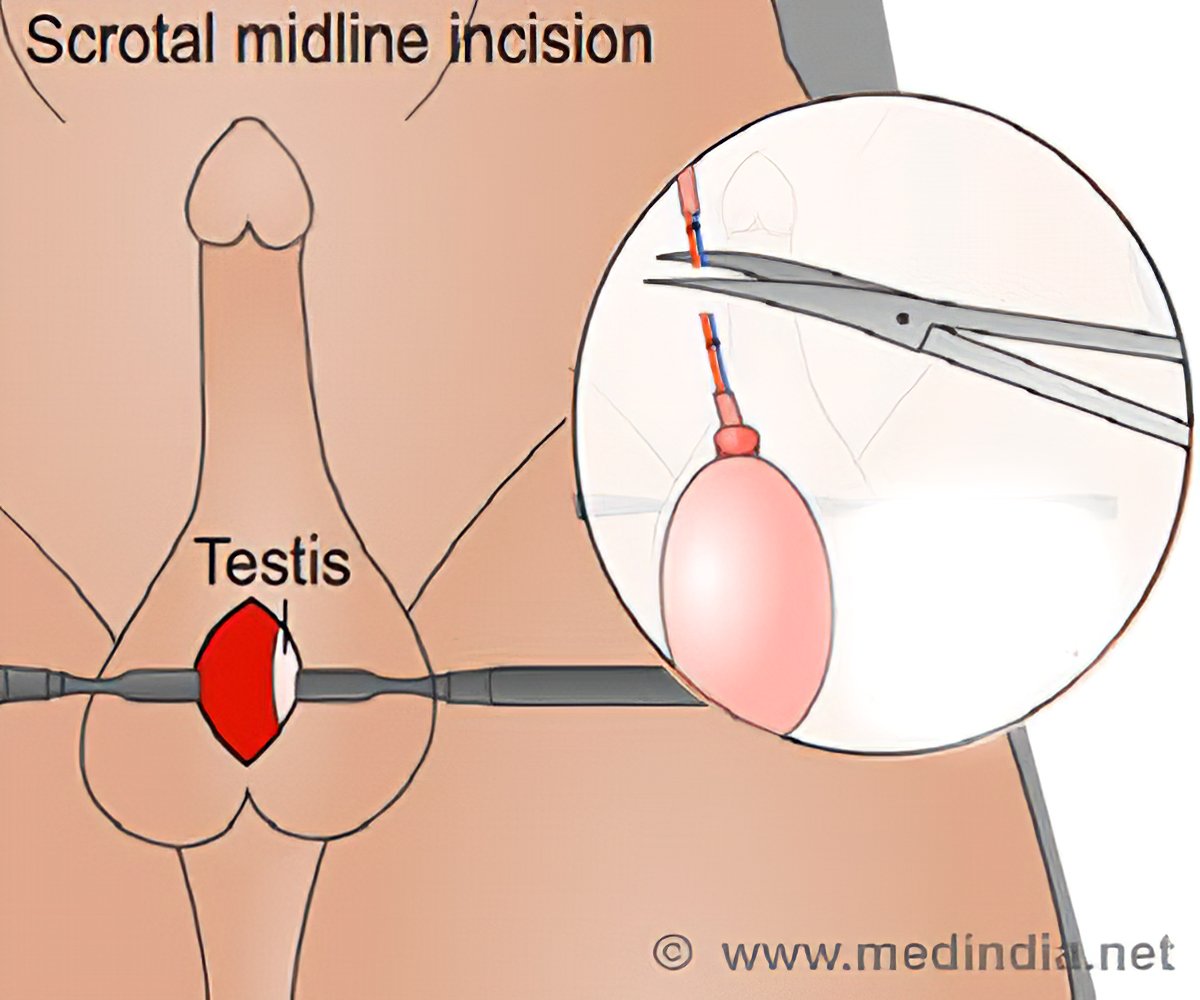
Surgical Castration

Chemical Castration - an overview | ScienceDirect Topics

Chemically Castrating: How It Works, Uses, and Side Effects
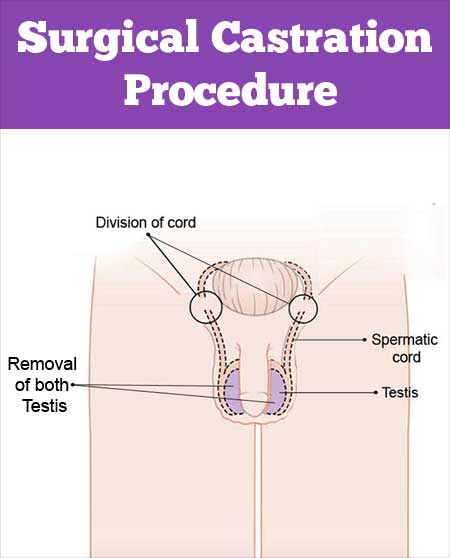
Surgical Castration
Castration of Calves
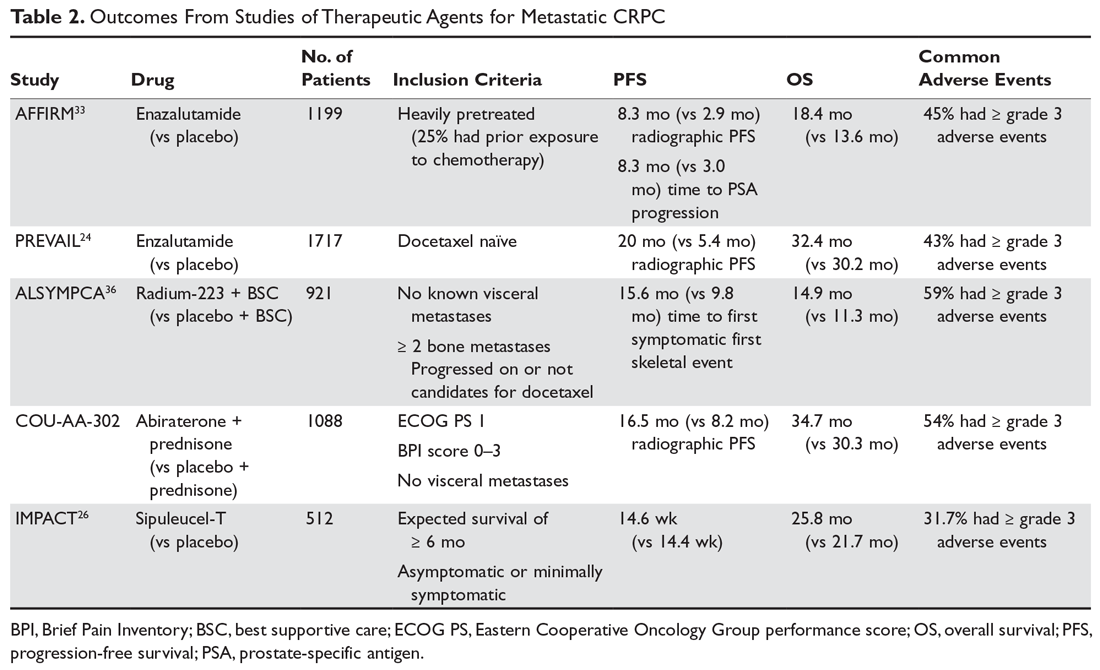
Management of Castration-Resistant Prostate Cancer | MDedge Hematology and Oncology
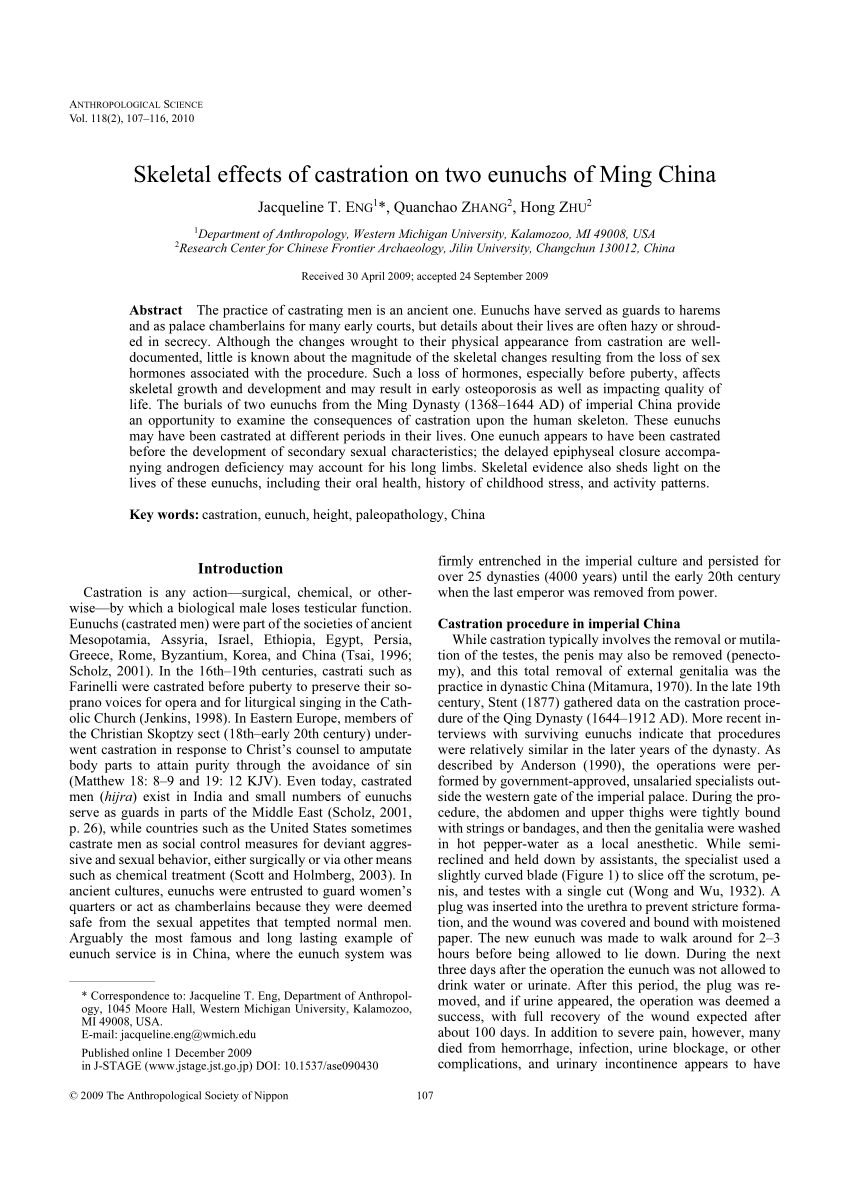
PDF) Skeletal effects of castration on two eunuchs of Ming China

Orchiectomy - Wikipedia

Chemical Castration and Contraception | Healthful Dog
Spay & Neuter Adverse Effects
Effects of Castration on the Life Expectancy of Contemporary Men - LessWrong
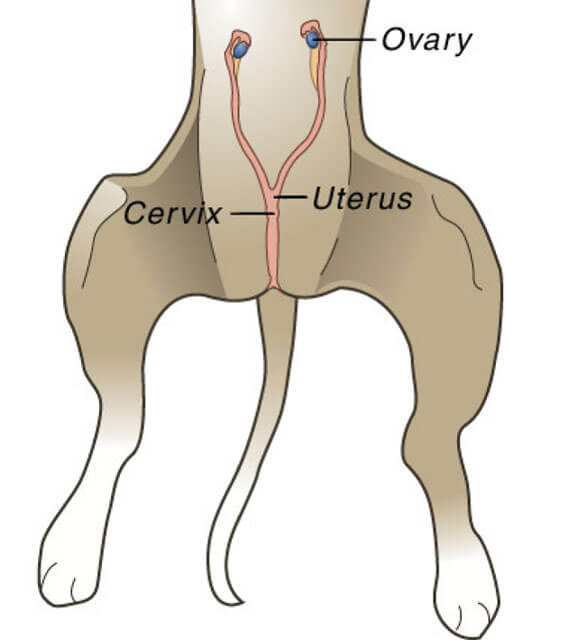
Dog Neutering: The Unspoken Risks Of Neutering | Dogs First
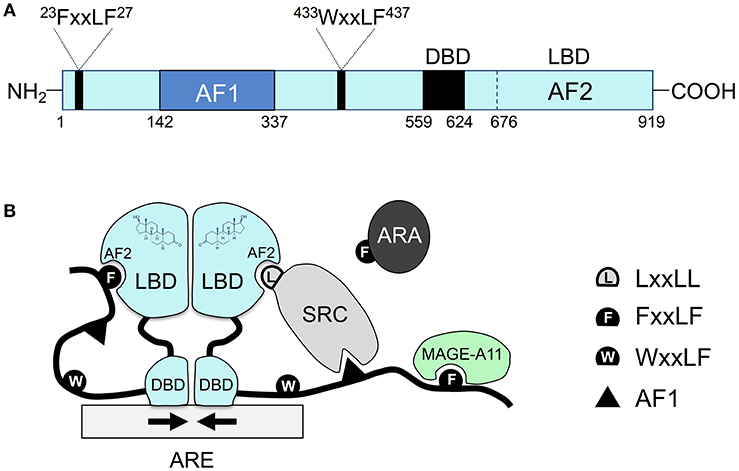
Frontiers | Androgen Receptor Signaling in the Development of Castration-Resistant Prostate Cancer | Oncology
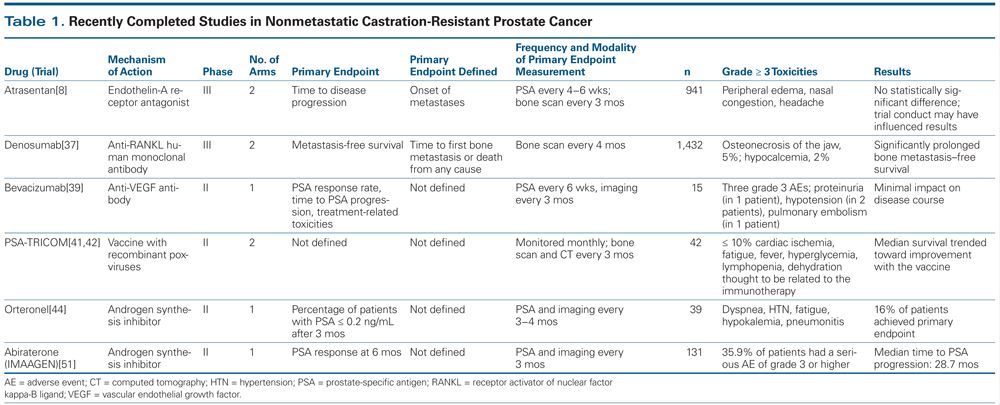
Treatment of Nonmetastatic Castration-Resistant Prostate Cancer

What It's Like to Be Chemically Castrated

The Evolving Treatment Landscape for Nonmetastatic Castration-Resistant Prostate Cancer
Why castrating lambs may not be helping your profits - Farming Independent

The castration effect | Wellcome Collection

Harvest, carcass, and subprimal yield traits of intact bulls and steers... | Download Table
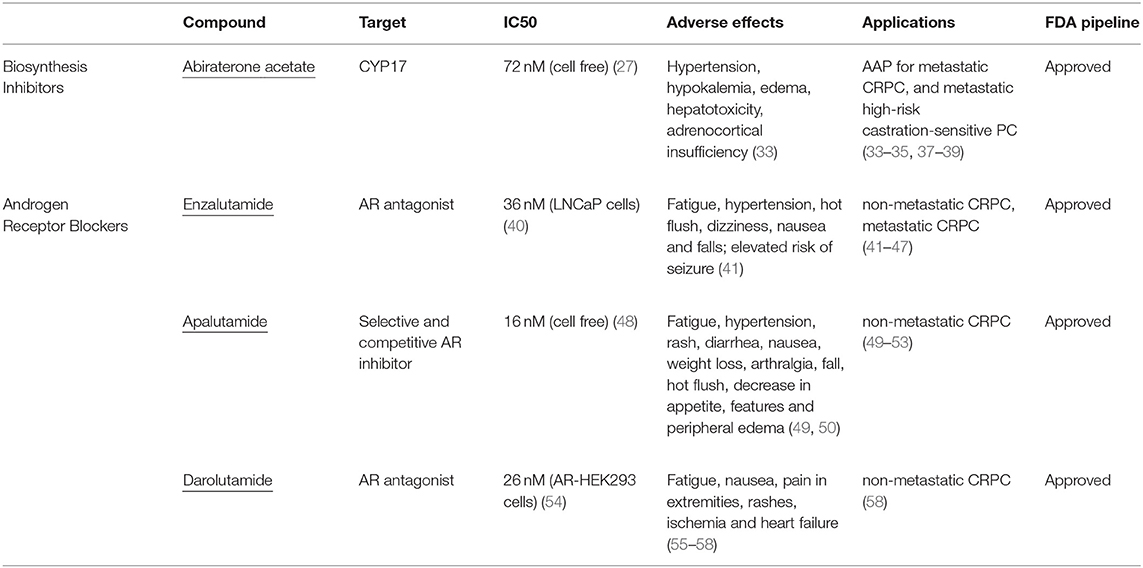
Frontiers | Second-Generation Antiandrogens: From Discovery to Standard of Care in Castration Resistant Prostate Cancer | Oncology
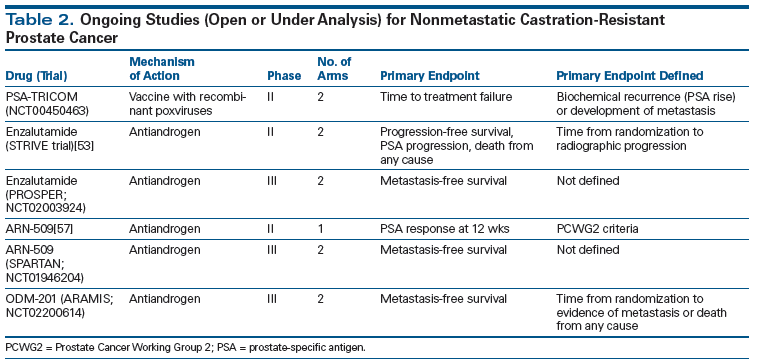
Treatment of Nonmetastatic Castration-Resistant Prostate Cancer
![Full text] Treatment of non-metastatic castration-resistant prostate cancer: focu | CMAR Full text] Treatment of non-metastatic castration-resistant prostate cancer: focu | CMAR](https://www.dovepress.com/cr_data/article_fulltext/s165000/165706/img/CMAR_A_165706_T0001.jpg)
Full text] Treatment of non-metastatic castration-resistant prostate cancer: focu | CMAR

Castration - Wikipedia
Economical impact of orchiectomy for advanced prostate cancer
Posting Komentar untuk "side effects of castration"